Understanding Gabapentin
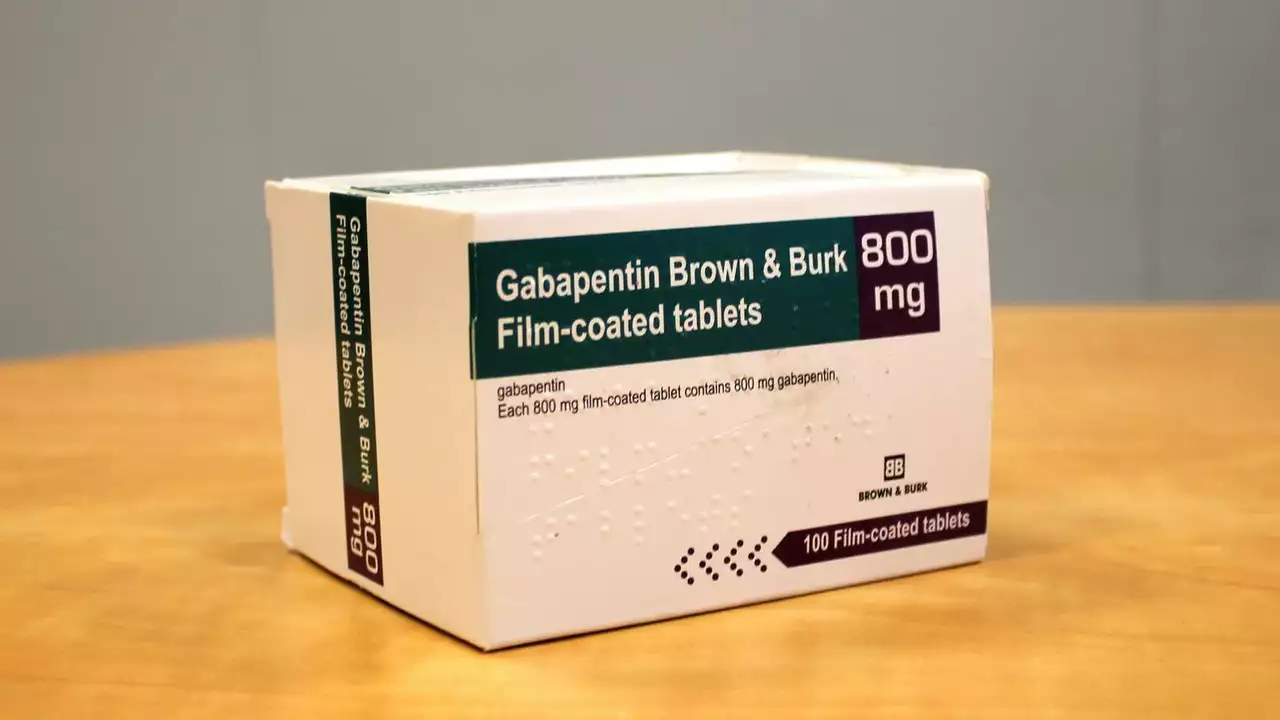
Before we delve into the specifics about gabapentin during pregnancy, it's important to understand what gabapentin is. Gabapentin is a medication primarily used to treat seizures and nerve pain. It's often prescribed for conditions such as epilepsy, restless leg syndrome, and postherpetic neuralgia. The drug works by calming down the nervous system and reducing the amount of pain signals that are sent out to the body.
The Use of Gabapentin During Pregnancy
Now, let's talk about the use of gabapentin during pregnancy. The safety of gabapentin during pregnancy is a topic of ongoing research. However, the current consensus among medical professionals is that it should be used with caution. This is largely due to the fact that there is limited data available on its safety during pregnancy, and some studies have suggested a potential risk of congenital malformations. It is important to note, however, that these studies are not definitive, and more research is needed to fully understand the potential risks.
Potential Risks of Gabapentin in Pregnancy
The potential risks of gabapentin during pregnancy are not fully understood, but some studies have suggested a possible link to congenital malformations. These risks are believed to be higher during the first trimester, when the baby's organs are developing. Other potential risks may include preterm birth and low birth weight. However, it's important to note that these risks are considered to be relatively rare, and the majority of women who take gabapentin during pregnancy do not experience these complications.
Precautions When Taking Gabapentin During Pregnancy
Given the potential risks, there are several precautions that should be taken if you are considering taking gabapentin during pregnancy. First, it's important to talk to your doctor about the potential risks and benefits. They can help you weigh the potential benefits of the medication against the potential risks. Second, it's important to monitor your baby closely for any signs of complications. This may involve regular ultrasounds and other tests to check the baby's development.
Alternatives to Gabapentin During Pregnancy
If you are uncomfortable with the potential risks of gabapentin during pregnancy, there are alternatives available. Other medications may be safer for use during pregnancy, or non-drug therapies may be effective. Again, it's important to discuss these options with your doctor to determine the best course of action for you and your baby.
Conclusion
In conclusion, while gabapentin can be an effective treatment for certain conditions, its use during pregnancy should be approached with caution. The potential risks, while relatively rare, are serious, and should be weighed carefully against the potential benefits. As always, the best course of action is to discuss your options with your doctor, who can provide you with the most up-to-date and accurate information.
Releted Post
21 Jul 2023


The article could benefit from clearer citation formatting.
While the author emphasizes caution, one must remember that the moral imperative to alleviate suffering often outweighs speculative teratogenic concerns; indeed, depriving pregnant patients of effective neuropathic pain relief may constitute an ethical lapse. Moreover, the paucity of conclusive data should not be wielded as a pretext for blanket prohibition, as such a stance neglects the nuanced principle of beneficence. It would be remiss to ignore the substantial body of clinical experience indicating acceptable outcomes when gabapentin is judiciously prescribed. In light of these considerations, a more balanced perspective-one that weighs both potential risk and undeniable therapeutic advantage-should be advocated.
I completely understand the anxiety that many expectant mothers feel when confronted with the prospect of taking any medication, especially one that is not explicitly labeled as safe for pregnancy.
Your article does a solid job of laying out the current state of research, and I appreciate the balanced tone that acknowledges both the limited data and the potential benefits.
That being said, it is absolutely crucial to recognize that the fear of unknown risks should not automatically translate into a blanket refusal to treat legitimate pain.
When a woman suffers from severe neuropathic pain, the physiological stress alone can jeopardize fetal development, and in such cases, the therapeutic advantage of gabapentin may far outweigh the theoretical danger.
Furthermore, the studies you cite, while not definitive, do not demonstrate a dramatic spike in congenital malformations, which suggests that the drug’s teratogenic profile is, at best, modest.
It is also worth noting that many clinicians have amassed years of practical experience using gabapentin safely in pregnant patients, and their anecdotal evidence should not be dismissed lightly.
In addition, the article could have benefited from a deeper discussion of dose–response relationships, because lower doses might mitigate any residual risk while still providing adequate pain control.
Patients should be encouraged to engage in a thorough, shared‑decision‑making process with their obstetrician and neurologist, weighing the precise severity of their symptoms against the modest, albeit uncertain, risks highlighted in the literature.
I would also argue that a proactive monitoring plan-such as regular ultrasounds and growth assessments-can further reduce any potential negative outcomes.
This approach not only empowers the patient but also creates a safety net that satisfies both the medical team’s caution and the mother’s need for relief.
Moreover, the narrative surrounding ‘caution’ should not be conflated with ‘paralysis’, as too much hesitancy can lead to undertreated pain, which carries its own set of maternal and fetal complications.
Your conclusion rightly calls for more research, yet in the meantime, clinicians must rely on the best available evidence combined with clinical judgment.
In practice, this often means that gabapentin, when prescribed at the lowest effective dose and accompanied by vigilant monitoring, is a reasonable option for many pregnant patients.
I also think it would be helpful to mention alternative non‑pharmacologic therapies, such as physiotherapy and cognitive‑behavioral techniques, as adjuncts that can further lower the necessary drug dose.
Overall, the article strikes a commendable balance, but a stronger emphasis on individualized care plans would make it even more useful for both providers and patients.
In short, while caution remains warranted, an outright refusal to consider gabapentin ignores the complex reality of pain management during pregnancy.
Look, we American doctors have been pioneering pain management for decades, and it’s laughable that overseas guidelines try to dictate what we should or shouldn’t prescribe to our own mothers. The data on gabapentin isn’t some conspiratorial plot; it’s simply a matter of weighing real‑world outcomes that our hospitals have tracked for years. If you want to throw caution to the wind, fine, but don’t pretend that the U.S. health system is some weak‑link that needs foreign moral policing.
Honestly, I cant believe people still act like they dont know the basics about meds in pregancy – it’s practically common sense, especially if you grew up in the US where we have the best guidelines. The goverment has already put out clear advisories, so you dont need to keep re‑hashing the same old fears. And yeah, i get that some folks think they’re being polite by asking “what do you think?” but honestly, it’s just a way to avoid taking responsibility for their own health choices. Stop over‑thinking and trust the experts, they’ve been doing this for years.
hey folks, just wanted to drop a quick note – if you’re pregnant and considering gabapentin, definitely talk to your OB‑GYN first. i’ve seen a lot of cases where a low dose helped a mom get some relief without any noticeable issues. keep an eye on any weird symptoms and get regular ultrasounds, that way you and the doc can catch anything early. also, don’t forget about non‑drug options like physio or CBT, they can cut down the amount you need to take. hope that helps!
The piece, while informative, suffers from a lack of statistical rigor; it presents anecdotal observations without quantifying incidence rates, which undermines its credibility. Moreover, the recommendation to “discuss with your doctor” is overly generic and fails to provide actionable guidance for clinicians faced with complex risk‑benefit analyses. A more thorough appraisal of the existing literature, complete with confidence intervals and meta‑analytic findings, would have elevated the discourse substantially.