Brand Drug Production Costs: What Really Goes Into Making Prescription Medicines
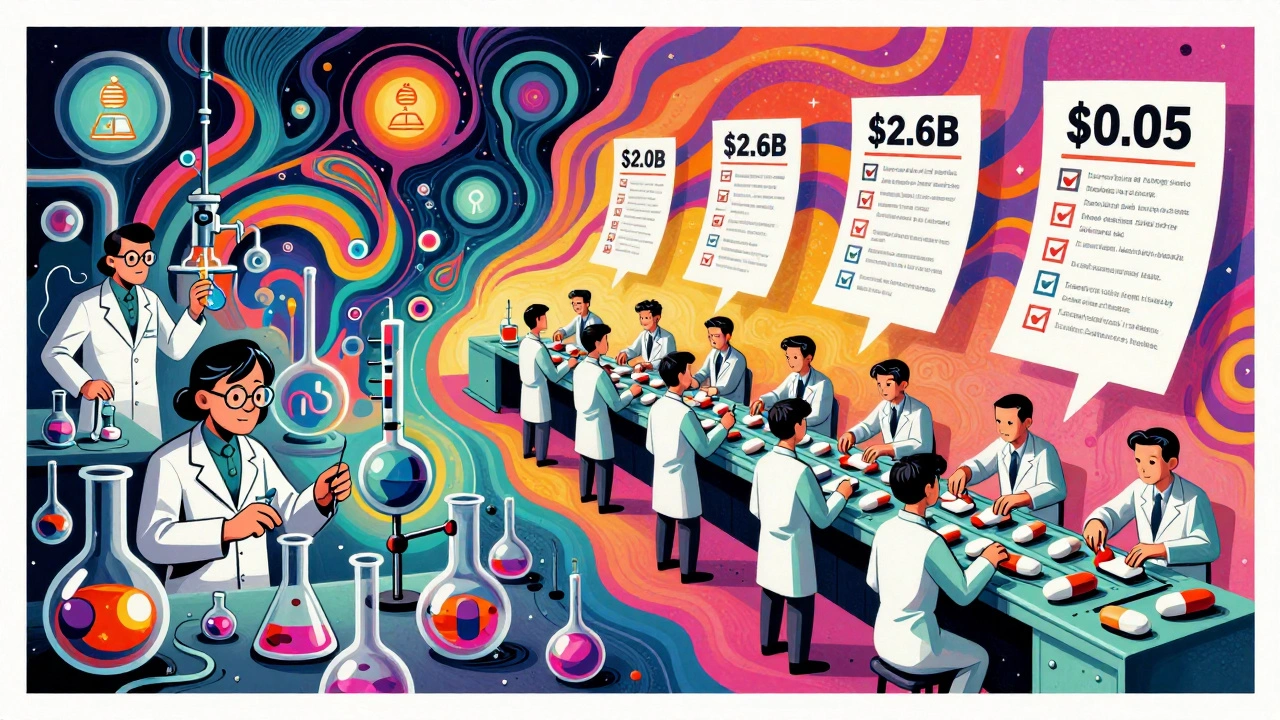
When you see a $500 pill on the pharmacy shelf, you’re not just paying for the chemical inside—you’re paying for brand drug production costs, the full expense of developing, testing, patenting, and marketing a new medicine over decades. Also known as pharmaceutical R&D investment, this includes everything from lab research to clinical trials, regulatory filings, and even the cost of failed drugs that never made it to market. Most people assume drug companies charge high prices because they’re greedy. But the truth is more complex: the average cost to bring a single new drug to market is over $2.6 billion, according to independent studies from the Tufts Center for the Study of Drug Development. That number includes losses from the 90% of drugs that fail during testing.
Behind every brand drug is a long chain of expenses: patent protection, manufacturing facilities built to FDA standards, quality control labs, and marketing teams that convince doctors to prescribe it. And then there’s the authorized generics, when the original brand manufacturer produces its own generic version to keep market share after the patent expires. These aren’t cheap knockoffs—they’re identical pills sold under a different label, often at prices higher than true generics because they still carry the brand’s reputation. This strategy lets companies profit even as competitors enter the market. Meanwhile, the pharmaceutical manufacturing, the actual process of turning raw chemicals into pills, injections, or creams. Also known as drug formulation, it requires sterile environments, precision equipment, and trained staff to meet global standards like ICH guidelines. It’s not just mixing powders—it’s controlling temperature, humidity, and contamination at every step. One mistake can lead to a nationwide recall, like those seen in recent FDA alerts.
Why does this matter to you? Because understanding these costs helps explain why some medications stay expensive even after generics exist. It also shows why some patients pay more for a brand drug than a generic—even when they’re made by the same company. The real story isn’t about profit margins alone. It’s about risk, regulation, and the hidden infrastructure behind every pill you swallow.
Below, you’ll find real-world examples of how drug makers manage these costs, what happens when patents expire, and how government policies like the Hatch-Waxman Act shape what you pay at the counter. You’ll also see how bioavailability studies, genetic testing, and international standards all tie into the bigger picture of drug pricing and safety. This isn’t theory—it’s what’s happening in labs, factories, and pharmacies right now.
Generic drugs cost far less than brand-name drugs not because they're made cheaper, but because labor costs are lower due to scale, outsourcing, and simplified processes. Here's how production labor differs between the two.