Drug Cost Breakdown: Understand What You're Really Paying For
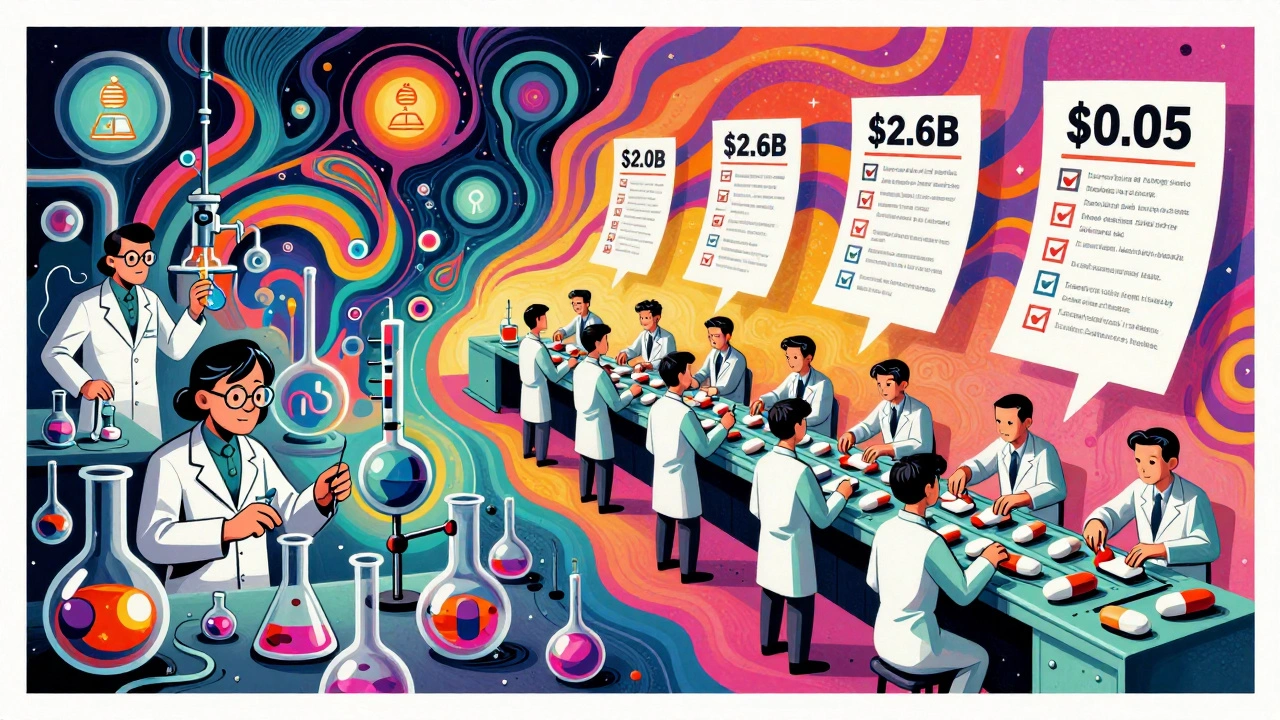
When you pick up a prescription, the price tag doesn’t tell the whole story. A drug cost breakdown, the detailed analysis of how a medication’s final price is formed, including manufacturing, distribution, branding, and retail markups. Also known as pharmaceutical pricing structure, it shows why two identical pills can cost wildly different amounts depending on where you buy them. Most people assume the price reflects the cost of making the drug. It doesn’t. The active ingredient in a generic pill might cost pennies. What you’re paying for is often the packaging, the brand name, the pharmacy’s markup, and layers of middlemen between the factory and your hands.
Take authorized generics, brand-name drugs sold under a different label by the same manufacturer after patent expiry. Also known as brand generic, these are chemically identical to the original but priced higher than traditional generics because they carry the brand’s reputation—and patients often pay more out of habit. Then there’s the Pharmaceutical Benefits Scheme, Australia’s government program that caps what patients pay for prescription drugs. Also known as PBS Australia, it shows how public policy can directly lower drug costs for millions—something the U.S. system rarely does. In the U.S., you’re at the mercy of pharmacy benefit managers, insurance networks, and patent extensions that delay cheaper alternatives. The Hatch-Waxman Act, the 1984 law that created the modern generic drug pathway. Also known as Drug Price Competition and Patent Term Restoration Act, it was meant to speed up affordable access. But loopholes let manufacturers extend monopolies through minor reformulations or dosing patents, keeping prices high. Meanwhile, bioavailability studies ensure generics work the same as brands, but that doesn’t stop pharmacies from charging more for the name you recognize.
It’s not just about the pill. A drug cost breakdown includes the cost of patents, legal battles over exclusivity, marketing campaigns, and even how insurers negotiate rebates behind closed doors. The same drug might be cheaper in Australia because the government negotiates bulk prices. In the U.S., the same drug could be priced differently at CVS, Walmart, or a local pharmacy based on their contracts. And don’t forget the hidden fees—dispensing charges, insurance copays, and mandatory counseling fees that get tacked on without warning.
You don’t need to be a pharmacist to understand this. You just need to know where to look. The next time you see a high price, ask: Is this the actual cost of the medicine—or just the cost of the system around it? Below, you’ll find real examples of how drug pricing works, who profits, and how to spot when you’re being overcharged. Some posts show you how to find cheaper alternatives. Others reveal how big pharma plays the system. And one even explains why your doctor’s prescription might cost more than the generic you could buy next door—if you knew where to look.
Generic drugs cost far less than brand-name drugs not because they're made cheaper, but because labor costs are lower due to scale, outsourcing, and simplified processes. Here's how production labor differs between the two.