Familial hypercholesterolemia (FH): what to watch for and what to do
If your LDL cholesterol is very high even though you eat well and exercise, FH could be the reason. Familial hypercholesterolemia is an inherited condition that raises LDL from birth and greatly increases the risk of early heart disease. This page helps you spot the signs, get the right tests, and understand treatment options so you can act fast.
How to suspect FH
Look for these red flags: LDL cholesterol above 190 mg/dL in adults (much higher in some cases), heart attack at a young age in you or close relatives, or cholesterol deposits in the tendons (xanthomas) or around the eyelids (xanthelasma). About 1 in 250 people have FH in its heterozygous form — it’s common enough that doctors should think about it when LDL is very high.
If several family members have high cholesterol or early heart disease, tell your doctor. That family pattern is a key clue and means your relatives might need testing too.
Testing, diagnosis, and what comes next
Start with a fasting lipid panel to measure LDL. Doctors use clinical criteria (like the Dutch Lipid Clinic Network or Simon Broome criteria) plus family history to decide if genetic testing is helpful. Genetic testing can confirm mutations in genes such as LDLR, APOB, or PCSK9, but a negative test doesn’t rule out FH — the clinical pattern still matters.
Once FH is suspected or confirmed, family (cascade) screening is vital. That means testing parents, children, and siblings so you can catch high LDL early. Children with FH benefit from early lifestyle advice and, in many cases, starting treatment in childhood to prevent decades of arterial damage.
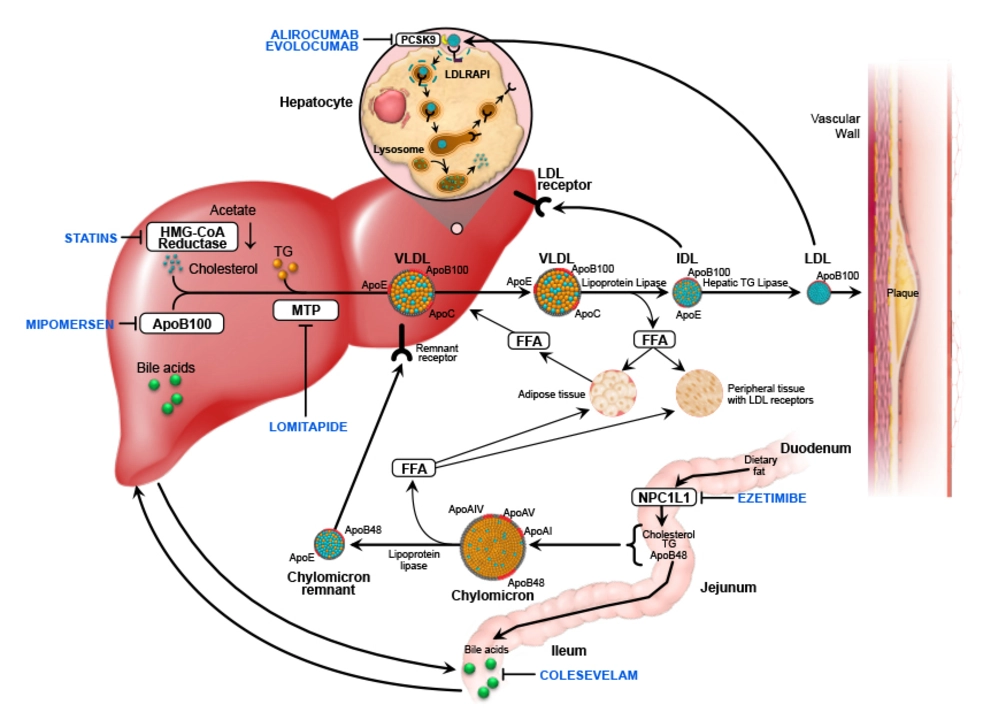
Treatment mixes powerful medicines and lifestyle steps. High-intensity statins are the mainstay and often started right away. If LDL remains high, doctors add ezetimibe and, for many people, PCSK9 inhibitors or newer drugs to lower LDL further. Lifestyle still matters: healthy food, regular activity, quitting smoking, and maintaining a healthy weight help but usually won’t replace medication for FH.
Monitor treatment with repeat lipid panels and basic liver tests as your doctor recommends. Women who are pregnant or plan pregnancy need a special plan because many cholesterol drugs aren’t safe in pregnancy; discuss timing and alternatives with your clinician.
Don’t wait to act. FH causes lifelong high LDL and raises heart disease risk decades earlier than normal. If you or your family has strong cholesterol or heart disease history, ask your doctor about FH, get tested, and start a treatment plan. Early detection changes the outcome.
As a blogger, I recently came across an interesting topic regarding the role of Fenofibrate in treating Familial Hypercholesterolemia (FH). FH is a genetic disorder that leads to dangerously high cholesterol levels, increasing the risk of heart disease. Fenofibrate, a medication commonly used to lower cholesterol, has shown promise in managing this condition. It works by reducing the production of triglycerides and increasing the removal of cholesterol from the bloodstream. In conclusion, Fenofibrate appears to be a valuable tool in the fight against Familial Hypercholesterolemia, offering potential benefits to those affected by this challenging disorder.