Understanding Familial Hypercholesterolemia and Its Impact on Health
Familial Hypercholesterolemia (FH) is a genetic disorder that causes high levels of low-density lipoprotein cholesterol (LDL-C) in the blood. This condition affects approximately 1 in 250 people worldwide and can lead to premature cardiovascular disease if left untreated. As someone who has dealt with this disorder, I understand the importance of finding effective treatments to manage and control FH. In this article, I will discuss the role of Fenofibrate, a medication that has shown promise in treating Familial Hypercholesterolemia.
Fenofibrate: What Is It and How Does It Work?
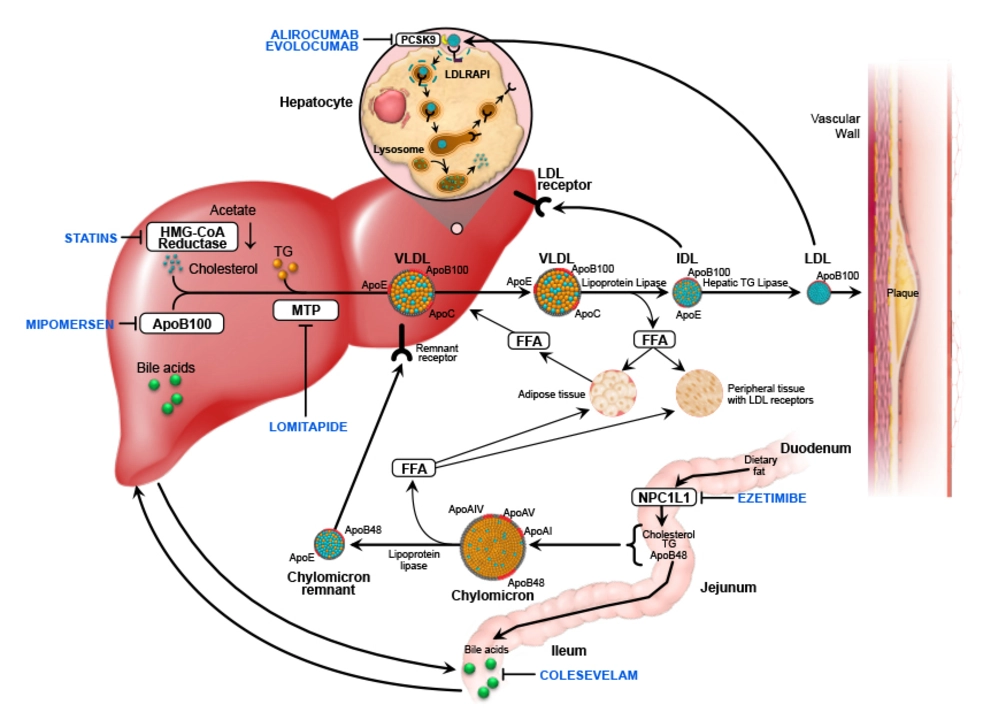
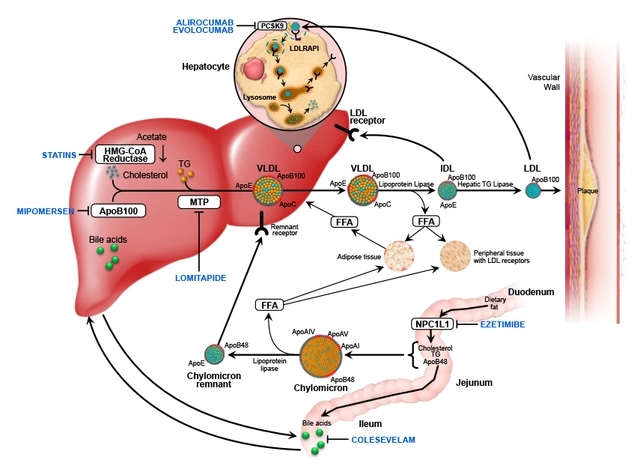
Fenofibrate is a type of medication known as a fibrate. It works by reducing the production of triglycerides in the liver and increasing the breakdown of lipoprotein particles in the blood. This helps lower LDL-C levels, which is crucial for managing FH. Additionally, Fenofibrate has been shown to increase high-density lipoprotein cholesterol (HDL-C), also known as the "good" cholesterol, which can help protect against cardiovascular disease. As a patient with FH, I have found that incorporating Fenofibrate into my treatment plan has significantly improved my cholesterol levels and overall heart health.
The Benefits of Fenofibrate in Treating Familial Hypercholesterolemia
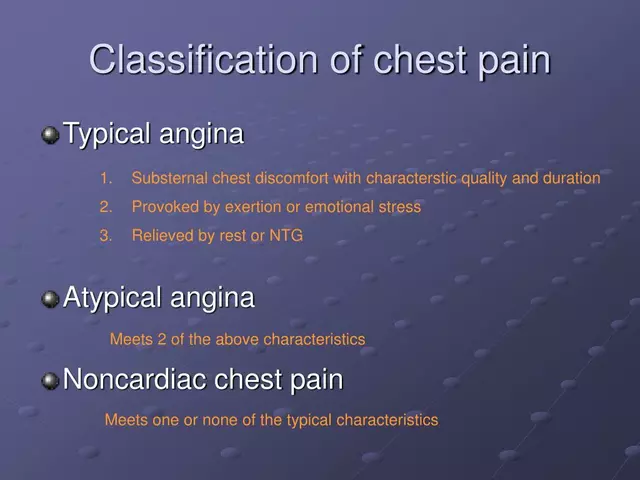
There are several benefits to using Fenofibrate as part of a comprehensive treatment plan for Familial Hypercholesterolemia. The most significant benefit is its ability to lower LDL-C levels, which are a primary concern for individuals with FH. By reducing these levels, Fenofibrate can help slow down the progression of atherosclerosis, a condition in which plaque builds up in the arteries and increases the risk of heart attack and stroke. Furthermore, Fenofibrate has been shown to improve other lipid parameters, such as increasing HDL-C levels and lowering triglycerides, which can contribute to better overall cardiovascular health.
Combining Fenofibrate with Other Cholesterol-Lowering Medications
In many cases, Fenofibrate may be used in combination with other cholesterol-lowering medications, such as statins, to achieve optimal lipid control in patients with Familial Hypercholesterolemia. This is because different medications work through different mechanisms to lower cholesterol levels, and combining them can lead to more significant reductions in LDL-C. As a patient with FH, I have experienced the benefits of this combination therapy firsthand. By taking both Fenofibrate and a statin, I have been able to achieve better control over my cholesterol levels and reduce my risk of cardiovascular events.
Side Effects and Precautions of Fenofibrate
As with any medication, there are potential side effects associated with Fenofibrate use. Some common side effects include headache, back pain, gastrointestinal issues, and respiratory symptoms. While these side effects are generally mild and manageable, it is essential to discuss them with your healthcare provider if they become bothersome. Additionally, there are some precautions to consider when taking Fenofibrate. It is important to have regular blood tests to monitor liver function and lipid levels while on this medication, as there is a risk of liver damage in rare cases. As an FH patient, I have experienced some mild side effects, but the benefits of Fenofibrate far outweigh these concerns for me.
Discussing Fenofibrate with Your Healthcare Provider
Before starting Fenofibrate or any new medication, it is crucial to have an in-depth discussion with your healthcare provider about the potential risks and benefits. They will be able to determine if Fenofibrate is appropriate for your specific situation, based on your medical history, current medications, and overall health. As someone with Familial Hypercholesterolemia, I found that working closely with my healthcare provider and having open conversations about my treatment options allowed me to make informed decisions about my care and ultimately led to better health outcomes.
Conclusion: Fenofibrate as a Valuable Tool in Managing Familial Hypercholesterolemia
In conclusion, Fenofibrate is a valuable tool in the management of Familial Hypercholesterolemia. Its ability to lower LDL-C levels, improve other lipid parameters, and reduce the risk of cardiovascular disease makes it an essential part of a comprehensive treatment plan for individuals with FH. As a patient living with this genetic disorder, I can attest to the benefits of incorporating Fenofibrate into my treatment regimen. By working closely with my healthcare provider and using this medication in conjunction with other cholesterol-lowering therapies, I have been able to achieve better control over my cholesterol levels and improve my overall heart health.

The pharmacokinetic profile of fenofibrate hinges on PPAR‑α activation, which modulates hepatic lipase activity. By up‑regulating the expression of APOA1, fenofibrate can augment HDL‑C synthesis, an effect especially relevant in FH patients 😊. Moreover, the drug’s impact on triglyceride hydrolysis complements statin therapy, offering a synergistic lipid‑lowering regimen. Clinical data suggest a modest yet statistically significant reduction in LDL‑C when combined with high‑intensity statins.
Oi mate, this fenofibrette thingy is a bloody game changer, defintely the best thing since fish 'n chips in the UK! It smashes those nasty triglyciders and shoves the bad cholestrol right outta your arteries, innit? No more heart attacks for us Brits-cheers to that!
It is essential to clarify that fenofibrate does not replace statins; it serves as an adjunctive agent. The peer‑reviewed literature consistently reports a 5–10 % reduction in LDL‑C when fenofibrate is added to a statin regimen. Patients must be monitored for hepatic transaminases, as omission of this safety check would be medically irresponsible. Therefore, adherence to guideline‑directed therapy remains paramount.
That’s a solid summary, though the liver enzymes rise is pretty rare. I’ve seen most folks tolerate fenofibrate just fine, but a quick blood check every few months never hurts. Also, the drug’s half‑life can vary a bit-just a heads‑up.
It’s nice to see the community discussing adjuncts, even if some people act like fenofibrate is a miracle cure-yeah, right, as if it were a magic pill. Still, the combination does give those on statins a bit of extra mileage, so kudos for trying something beyond the usual.
Honestly, many folks in India overlook the importance of diet alongside medicine, which is a huge mistake. Fenofibrate can help, but without proper nutrition it’s just a band‑aid. Also, the drug is sometimes misprescribed, leading to unnecessary side‑effects.
When considering fenofibrate for familial hypercholesterolemia, it is crucial to evaluate both the biochemical mechanisms and the real‑world patient experiences. The drug acts primarily as an agonist of peroxisome proliferator‑activated receptor alpha, leading to increased catabolism of triglyceride‑rich lipoproteins and a modest rise in high‑density lipoprotein particles. This biochemical cascade can indirectly influence low‑density lipoprotein concentrations by shifting the lipid equilibrium toward a less atherogenic profile. In clinical trials, patients receiving fenofibrate alongside statins demonstrated an average LDL‑C reduction of approximately eight percent, which, while not dramatic, is statistically meaningful in a high‑risk cohort. Moreover, the improvement in HDL‑C, often ranging from ten to fifteen percent, contributes to a more favorable cholesterol ratio, a factor associated with reduced cardiovascular events.
However, the therapeutic effect is not uniform across all genotypes of FH; certain LDL‑R mutations may blunt the response, necessitating personalized dosing strategies. Side‑effects such as mild gastrointestinal discomfort and transient elevations in serum creatinine have been reported, but these are generally manageable with dose adjustments. Regular monitoring of liver function tests and renal parameters remains a cornerstone of safe fenofibrate therapy, and most patients tolerate the regimen well over long periods. 😊
From a patient perspective, the addition of fenofibrate often translates to a tangible sense of control over one’s condition, especially when prior statin monotherapy failed to achieve target lipid levels. This psychological benefit should not be underestimated, as adherence tends to improve when individuals feel actively involved in their treatment plan.
Nevertheless, clinicians must remain vigilant about drug interactions, particularly with anticoagulants and certain antifungal agents, which can amplify the risk of adverse events. Education on lifestyle modifications-dietary saturated fat reduction, regular aerobic exercise, and smoking cessation-still forms the foundation upon which pharmacologic therapy builds. In summary, fenofibrate serves as a valuable adjunct in the multifaceted management of FH, offering incremental lipid improvements, a favorable safety profile, and enhanced patient empowerment when used judiciously.
Great overview-thanks for breaking it down so clearly.
It’s fascinating how the pharmaceutical industry pushes fenofibrate as the next‑big thing in cholesterol control, almost as if they’re trying to distract us from the real issue: the hidden agenda behind diet‑labeling regulations. The studies that highlight its benefits are often funded by companies with a vested interest, which makes you wonder what they’re not telling us about long‑term safety. I’ve read that some labs manipulate trial data to downplay rare but serious liver events, a practice that would be unthinkable if the system were truly transparent. Still, many patients report feeling better, and that’s a genuine outcome we can’t ignore. The key is to stay informed, question the sources, and not accept every glossy press release at face value. Remember, a healthy lifestyle can’t be replaced by any pill, no matter how many “clinical trials” back it up. 🌐
Indeed, the data, while promising, should be examined critically, especially considering potential conflicts of interest, and patients, therefore, deserve full transparency, ongoing monitoring, and a balanced discussion of risks and benefits.
Fenofibrate is cheap and works well for many people.
While cost-effectiveness is a valid consideration, clinical efficacy must remain the primary criterion. 🙂
Oh, absolutely, because nothing screams “groundbreaking medical advancement” like a drug that merely nudges numbers a few points lower while we pretend it’s a miracle cure. The enthusiasm some patients display is almost adorable when you think about how many other lifestyle factors are being ignored in favor of a little pill. I mean, why bother with diet changes or exercise when you can pop a tablet and hope for the best? It’s not like the atherosclerotic process is multifactorial, right? And let’s not forget the endless stream of “success stories” that are probably cherry‑picked to keep the sales numbers up. Meanwhile, the real work-patient education, adherence to comprehensive therapy, and regular monitoring-gets shoved to the side. So yes, congratulations to fenofibrate for doing just enough to keep the hype alive, even if the actual impact on long‑term outcomes remains questionable. Cheers to incremental change!
Fenofibrate’s primary mechanism involves activation of PPAR‑α, which enhances fatty acid oxidation and reduces triglyceride synthesis. When combined with statins, it can provide an additive reduction in LDL‑C, typically in the range of 5‑10 %. Clinicians should monitor liver enzymes and renal function at baseline and periodically thereafter. Patient education on potential side‑effects, such as muscle pain or gastrointestinal upset, is essential for adherence.
The journey with fenofibrate can feel like painting a masterpiece with a palette of lipid‑lowering hues; each brushstroke of reduced triglycerides and lifted HDL‑C adds depth to the canvas of cardiovascular health. When you pair it with a statin, it’s like mixing bold primary colors-sudden, striking, and surprisingly harmonious. Of course, there are occasional splatters-minor side‑effects that remind us we’re dealing with chemistry, not magic. But with careful monitoring, the overall picture becomes vibrant and resilient, a testament to thoughtful, layered therapy.
In the grand tapestry of preventive medicine, fenofibrate represents a deliberate stitch that reinforces the weave of lipid management, reminding us that incremental advances, when applied with intention, can shape the destiny of cardiovascular outcomes. Therefore, embracing it as part of a holistic strategy is both prudent and necessary.