Understanding Angina and its Impact on Heart Health
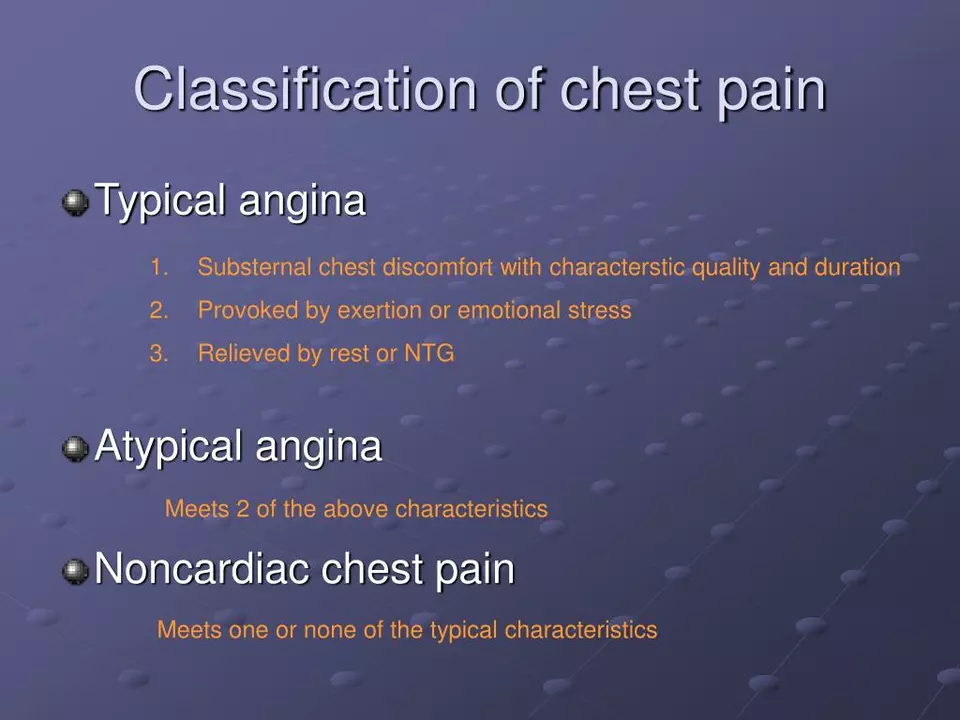
Angina is a common and sometimes debilitating condition that affects millions of people worldwide. It can cause intense chest pain and discomfort, often triggered by physical exertion or emotional stress. Angina occurs when the heart muscle doesn't receive enough oxygen-rich blood due to narrowed or blocked coronary arteries. This can lead to a variety of symptoms, including chest pain, shortness of breath, and fatigue. In this article, we will explore the connection between ivabradine and angina relief, and how this medication may provide an effective treatment option for those suffering from this condition.
The Role of Ivabradine in Treating Angina
Ivabradine is a medication that has recently gained attention for its potential to help those suffering from angina. It is a selective and specific inhibitor of the funny (I_f) current in the sinoatrial node, which is responsible for regulating heart rate. By inhibiting this current, ivabradine effectively slows down the heart rate, reducing the heart's oxygen demand and thus relieving angina symptoms.
How Ivabradine Works to Provide Angina Relief
The primary mechanism of action for ivabradine is its ability to slow down the heart rate. This is accomplished by inhibiting the I_f current in the sinoatrial node, which is the natural pacemaker of the heart. Slowing the heart rate allows the coronary arteries to supply more oxygen-rich blood to the heart muscle, reducing the oxygen demand and alleviating angina symptoms. Additionally, ivabradine has been shown to improve endothelial function, which can further improve blood flow to the heart muscle.
Studying the Effectiveness of Ivabradine in Clinical Trials
Numerous clinical trials have been conducted to evaluate the effectiveness of ivabradine in providing angina relief. Results from these studies consistently demonstrate that ivabradine is effective in reducing the frequency of angina attacks, improving exercise tolerance, and enhancing overall quality of life for patients with chronic stable angina. Furthermore, ivabradine has been shown to be well-tolerated, with a low incidence of side effects.
Comparing Ivabradine to Other Angina Treatments
When compared to other angina treatments, such as beta-blockers and calcium channel blockers, ivabradine has been shown to provide similar levels of symptom relief. However, ivabradine may be a more suitable option for certain patients, particularly those who cannot tolerate beta-blockers or calcium channel blockers due to side effects or contraindications. Additionally, ivabradine may be an effective add-on therapy for patients whose angina is not adequately controlled with other medications.
Considering Ivabradine for Heart Failure Patients
While the primary focus of this article is on the connection between ivabradine and angina relief, it is worth noting that ivabradine has also been approved for the treatment of certain types of heart failure. Research has shown that ivabradine can improve outcomes for patients with heart failure by reducing hospitalizations and improving quality of life. This further underscores the potential benefits of ivabradine for patients with cardiovascular conditions.
Understanding the Potential Side Effects of Ivabradine
As with any medication, ivabradine may be associated with certain side effects. Some of the most common side effects include bradycardia (slow heart rate), visual disturbances, and dizziness. Most side effects are mild and manageable, and patients should always discuss any concerns with their healthcare provider. It is also important to remember that the potential benefits of ivabradine in providing angina relief must be weighed against any potential risks or side effects.
Discussing Ivabradine with Your Healthcare Provider
If you or a loved one suffers from angina, it is important to discuss all treatment options with your healthcare provider. This includes the potential use of ivabradine as part of your angina management plan. Your healthcare provider can help determine if ivabradine may be an appropriate treatment option based on your individual needs, medical history, and current medications.
Conclusion: Ivabradine as a Promising Treatment for Angina Relief
In conclusion, ivabradine is a promising treatment option for patients suffering from angina. Its ability to slow the heart rate and improve blood flow to the heart muscle can provide significant relief from angina symptoms. Clinical trials have demonstrated its effectiveness in reducing angina attacks and improving overall quality of life, with a favorable safety profile. If you suffer from angina and are considering new treatment options, be sure to discuss the potential use of ivabradine with your healthcare provider.

Ivabradine sounds interesting.
This article nails it, but the tone is way too chill. I dont like the soft‑sell vibe, it feels like a sales pitch. Ivabradine does help but its not a silver bullet for all angina patients, as the author implies. Its still an add‑on, not a replacement for beta blockers. Get real, the side effects matter.
Let me dive deep into why ivabradine truly shines in the realm of angina therapy.
First, the drug’s selective inhibition of the funny current means it can decelerate heart rate without the negative inotropic effects seen with many beta‑blockers.
Secondly, patients who are intolerant to traditional agents often find relief thanks to ivabradine’s favorable side‑effect profile.
Clinical trials, such as the BEAUTIFUL study, have demonstrated a tangible reduction in angina frequency and an improvement in exercise tolerance.
Moreover, the drug enhances endothelial function, fostering better coronary blood flow.
From a physiological standpoint, slowing the pacemaker reduces myocardial oxygen consumption, directly addressing the ischemic mismatch that underlies angina.
This mechanism is especially valuable in patients with preserved ejection fraction where heart rate control is paramount.
In practice, we’ve observed that adding ivabradine to existing regimens can provide incremental symptom relief when monotherapy falls short.
The evidence also suggests a modest reduction in hospitalizations for heart failure, indicating broader cardiovascular benefits.
Patients should, however, be monitored for bradycardia, as excessive slowing can precipitate dizziness or syncope.
Visual disturbances, known as phosphenes, are a reported phenomenon but are typically reversible upon dose adjustment.
The drug’s pharmacokinetics allow for once‑daily dosing, which enhances adherence compared to multiple‑dose regimens.
Insurance coverage can be a hurdle, yet many formularies now include ivabradine given its proven efficacy.
It is essential for clinicians to evaluate comorbidities; for example, patients with severe atrial fibrillation may not benefit due to the drug’s atrial‑node specificity.
Overall, ivabradine offers a compelling adjunct for a subset of angina patients, bridging a therapeutic gap left by traditional agents.
In the grand scheme, its role is not to replace but to complement, providing a nuanced approach to ischemic heart disease management.
The author presents a biased overview, glossing over critical trial limitations. Methodological flaws, such as underpowered sub‑analyses, are omitted. Additionally, the safety discussion is superficial, ignoring real‑world adverse event frequencies. This piece reads more like a promotional brochure than a balanced review. Readers deserve a more rigorous assessment.
While your concerns are noted, the evidence base for ivabradine is not as flimsy as suggested. Multiple large‑scale studies have adhered to robust endpoints, and the reported side‑effects are comparable to existing therapies. Dismissing the data outright undermines scientific discourse.
Ivabradine is just another pharma cash cow, pushing meds onto vulnerable patients. They ignore cheaper lifestyle changes that could reduce angina without side effects.
While it's important to consider non‑pharmacological options, ivabradine offers a targeted mechanism that lifestyle alone cannot achieve for everyone. The drug’s ability to lower heart rate without affecting contractility makes it a valuable tool, especially for patients who cannot tolerate beta‑blockers. Balancing medication with lifestyle changes yields the best outcomes.
Ivabradine: effective, well‑tolerated, useful for select patients, adds value to therapy, consider it when beta‑blockers fail.
Great read! 😊 Ivabradine really seems like a promising option for those struggling with angina. 👍
Did you know Big Pharma is secretly funding all these studies? The whole thing is a ploy to keep us dependent on pills.
Conspiracy theories aside, the data from peer‑reviewed journals still stands. Trust the science.
Hey folks! 🎉 Let’s celebrate that ivabradine gives us another arrow in the quiver against angina. It’s especially handy for patients who can’t handle beta‑blockers. Remember, every heart is unique, so personalized care is key. Keep sharing insights and stay healthy!
Interesting discussion! 🤔 I’m curious how many clinicians are actually prescribing ivabradine in primary care settings.
From what I’ve seen, its use is growing, especially in specialized cardiology clinics where nuanced heart‑rate management is paramount.
People need to stop romanticizing drugs. Ivabradine is just another pill, not a miracle cure.
While I appreciate the caution, the evidence suggests ivabradine offers real benefit for a subset of patients, particularly those intolerant to other agents.
It is imperative to evaluate each therapeutic option within the broader context of cardiovascular risk reduction, ensuring that patient autonomy and informed consent remain paramount.
Our country's doctors should prioritize native remedies over foreign pharmaceuticals like ivabradine.
In conclusion, ivabradine represents a nuanced advancement in angina management, meriting thoughtful integration into individualized treatment algorithms.