Generic vs Brand Drug Manufacturing: What Really Happens Behind the Scenes
When you choose a generic drug, a medication that contains the same active ingredient as a brand-name drug but is sold under a different name after the patent expires. Also known as non-brand medication, it is required by the FDA to work the same way in your body as the original. But here’s the twist: the company that made the brand-name drug often makes the generic version too. These are called authorized generics, exact copies of the brand drug produced by the original manufacturer and sold under a different label. They’re not cheaper because they’re made differently—they’re cheaper because they skip the marketing costs. But sometimes, they cost almost as much as the brand. Why? Because the original company still controls the supply.
The whole system runs on the Hatch-Waxman Act, a 1984 U.S. law that balanced patent protection for innovators with faster access to low-cost generics. Before this law, generics couldn’t get approved without repeating every single clinical trial the brand company did. Now, they just need to prove bioequivalence, the scientific process that shows a generic drug delivers the same amount of active ingredient into your bloodstream at the same rate as the brand. That’s done through blood tests measuring AUC and Cmax—numbers that tell regulators whether the generic will do the same job as the brand. No guesswork. No shortcuts. Just hard data.
But not all generics are created equal in the eyes of the public. Some people still think generics are "weaker" or made in shoddy factories. That’s not true. The same FDA inspectors check brand and generic plants. The same quality standards apply. The difference isn’t in how they’re made—it’s in who makes them and why. Some companies make generics to help patients save money. Others make them to keep profits flowing after the brand patent expires. And sometimes, the same pill sits in two different bottles with two different prices.
What you’ll find in the posts below are real stories from inside this system: how brand manufacturers quietly launch their own generics to stay in control, how bioavailability studies make sure a $5 pill works just like a $50 one, and why the Federal Circuit Court’s rulings can delay your access to cheaper medicine. You’ll see how authorized generics confuse consumers, why the Hatch-Waxman Act is still shaping drug prices today, and what happens when a company tries to stretch a patent just to block competition. This isn’t theory. It’s how your medicine gets to your shelf—and who really benefits when it does.
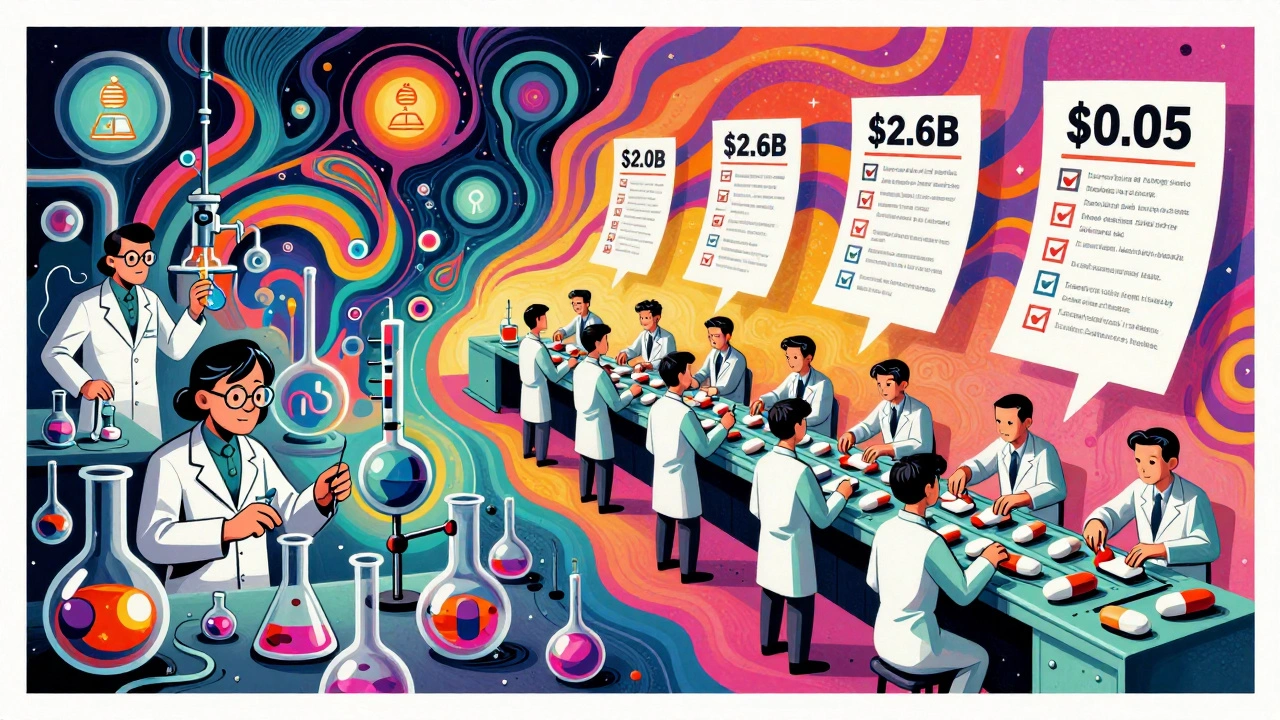
Generic drugs cost far less than brand-name drugs not because they're made cheaper, but because labor costs are lower due to scale, outsourcing, and simplified processes. Here's how production labor differs between the two.