Ivabradine: how it lowers heart rate and when it helps
Want to slow a fast heartbeat without changing blood pressure much? That’s the trick ivabradine pulls. Used mainly for certain types of heart failure and sometimes for stable angina, ivabradine cuts the heart rate by acting on the sinus node — the heart’s natural pacemaker. That makes it different from beta blockers.
How ivabradine works
Ivabradine blocks the funny current (If) in sinus node cells. Practically, that slows the resting heart rate without reducing how strongly the heart squeezes. For people with heart failure and a fast resting pulse, lowering heart rate can ease symptoms and reduce hospital visits when added to standard therapy. The drug is sold as Corlanor in many countries.
Typical candidates are adults with chronic heart failure with reduced ejection fraction who remain in normal sinus rhythm and have a resting heart rate of 70 bpm or higher despite the best tolerated dose of a beta blocker — or those who can’t tolerate beta blockers. Some regions also use ivabradine for chronic stable angina when heart rate control is needed.
Usual dosing and adjustments
Most adults start at 5 mg twice daily. If you’re 75 or older or have low body weight, a doctor might start at 2.5 mg twice daily. After two weeks your resting heart rate is checked: if it’s above 60 bpm, the dose can increase to 7.5 mg twice daily; if it’s 50–60 bpm, stay at the same dose; if it falls below 50 bpm or symptoms of bradycardia appear, the dose should be lowered or stopped. The maximum is 7.5 mg twice daily.
Take ivabradine with food at the same times each day. If you miss one dose, take it as soon as you remember unless it’s nearly time for the next dose. Don’t double up.
Safety first: don’t stop other heart meds without talking to your doctor. Always follow the cardiologist’s plan for dose changes and monitoring.
Common side effects include slow heart rate (bradycardia), a higher risk of atrial fibrillation, and unusual visual effects called phosphenes — brief, enhanced brightness or flashes of light. These visual effects usually go away on their own. Serious issues include very slow heartbeat, fainting, or irregular rhythm — seek care if they happen.
Ivabradine interacts with strong CYP3A4 inhibitors (like clarithromycin, ketoconazole) which can raise ivabradine levels and increase side effects. Avoid using those together. It’s also not for people with sick sinus syndrome, pronounced bradycardia, acute decompensated heart failure, severe hypotension, or pregnant women.
Practical tips: check your pulse at home, keep a list of all medicines to review for interactions, report dizziness or fainting, and get regular follow-ups with your cardiology team. If you’re unsure whether ivabradine fits your situation, ask a cardiologist — they’ll match the drug to your symptoms and other meds.
Ivabradine can be a useful tool when heart rate control matters but other options aren’t suitable. Used carefully and monitored, it helps many people feel better and avoid hospital visits.
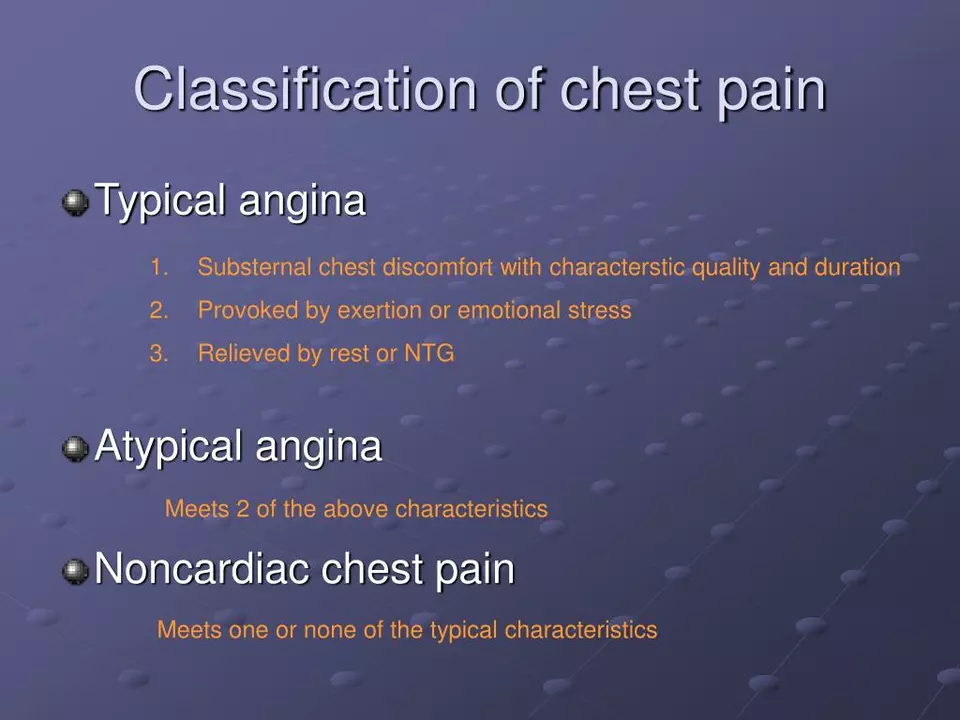
I recently came across an interesting study about the connection between Ivabradine and Angina relief. Ivabradine, a medication that reduces heart rate, has shown promising results in alleviating symptoms of angina. It works by slowing down the heart rate, allowing more time for blood flow and oxygen supply to the heart muscles. Many patients have experienced significant improvements in their quality of life after using this medication. I think it's fascinating how a simple change in heart rate can lead to such profound effects on a person's well-being.