Understanding Pneumonia and COPD
As someone who has experienced the challenges of living with chronic obstructive pulmonary disease (COPD), I know how important it is to understand the various factors that can contribute to the progression of this condition. One such factor is pneumonia, a common lung infection that can have serious consequences for individuals with COPD. In this article, we will explore the link between pneumonia and COPD, and discuss the implications of this connection for patients and their families.
The Increased Risk of Pneumonia in COPD Patients
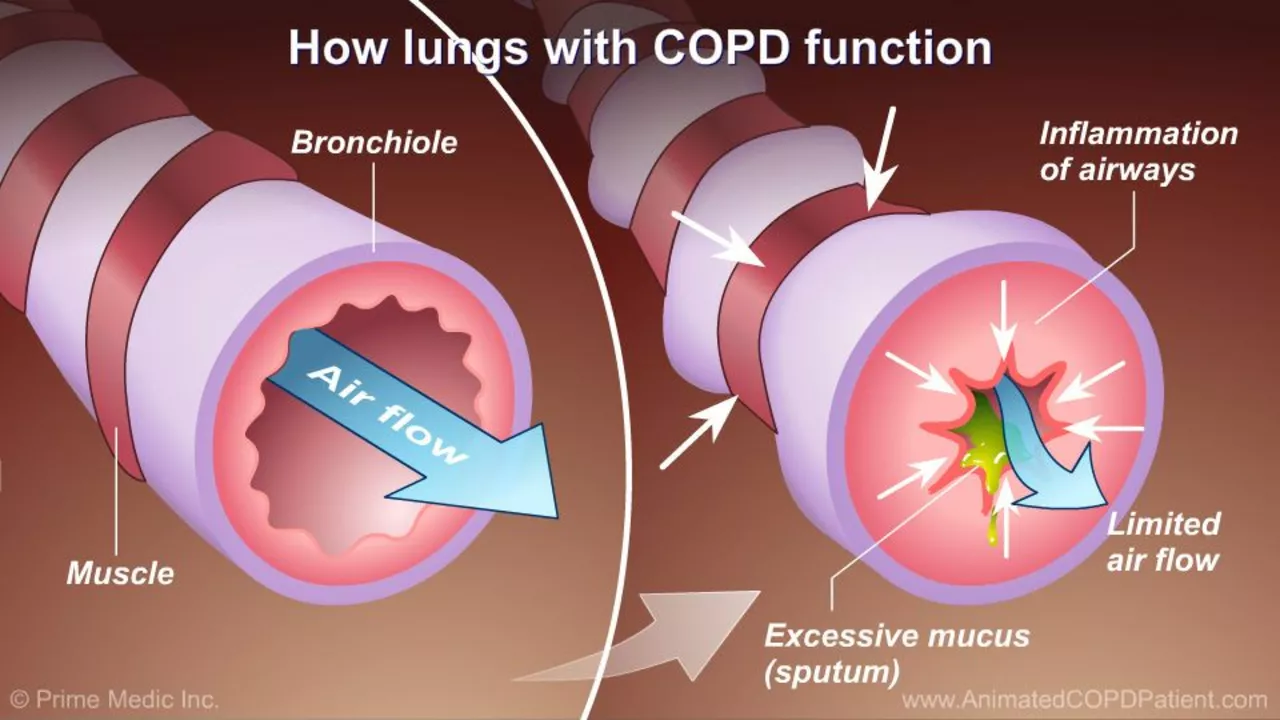
It is well-established that individuals with COPD are at a higher risk of developing pneumonia compared to the general population. This is because COPD weakens the respiratory system, making it more susceptible to infections. Furthermore, the inflammation and mucus production associated with COPD can create an environment that is conducive to bacterial growth, increasing the likelihood of pneumonia.
Additionally, many COPD patients also experience difficulty clearing mucus from their airways, which can further contribute to the risk of pneumonia. This is especially concerning because pneumonia can be a life-threatening condition, particularly for those with compromised lung function due to COPD.
Recognizing the Symptoms of Pneumonia in COPD Patients
Being able to recognize the symptoms of pneumonia is crucial for individuals with COPD, as early diagnosis and treatment can make a significant difference in the outcome. Some common symptoms of pneumonia include:
- Fever and chills
- Cough with mucus production
- Shortness of breath
- Chest pain
- Increased fatigue
- Confusion (especially in older adults)
If you or a loved one with COPD experiences these symptoms, it is essential to seek medical attention promptly to ensure appropriate treatment and minimize potential complications.
Preventing Pneumonia in Individuals with COPD
Given the increased risk of pneumonia in COPD patients, it is essential to take preventive measures to reduce the likelihood of developing this potentially dangerous infection. Some steps that can be taken to prevent pneumonia include:
- Getting vaccinated: There are vaccines available for both viral and bacterial pneumonia, which can help protect individuals with COPD from these specific infections.
- Practicing good hygiene: Washing your hands frequently and avoiding contact with individuals who have respiratory infections can help minimize the risk of pneumonia.
- Managing COPD: Taking prescribed medications, attending regular medical appointments, and practicing self-care can help keep COPD symptoms under control and reduce the risk of pneumonia.
- Quitting smoking: Smoking is a significant risk factor for both COPD and pneumonia, so quitting smoking is essential for reducing the risk of these conditions.
Treating Pneumonia in COPD Patients
If a COPD patient develops pneumonia, it is essential to begin treatment as soon as possible to minimize the risk of complications. Treatment for pneumonia typically involves the use of antibiotics, which are effective against bacterial infections. In some cases, antiviral medications may also be prescribed if the infection is caused by a virus.
Additionally, COPD patients with pneumonia may require supplemental oxygen to help maintain adequate oxygen levels in the blood. In severe cases, hospitalization may be necessary to provide more intensive care and monitoring.
Addressing the Emotional Impact of Pneumonia in COPD Patients
Dealing with pneumonia can be emotionally challenging for both the individual with COPD and their family members. The fear of complications and the potential impact on overall health can be overwhelming. It is essential to address these emotional concerns by seeking support from loved ones, engaging in open communication with healthcare providers, and considering professional counseling if needed.
Conclusion
Understanding the link between pneumonia and chronic obstructive pulmonary disease (COPD) is crucial for individuals living with this condition. By recognizing the symptoms of pneumonia, taking preventive measures, and seeking prompt treatment, COPD patients can minimize the risk of complications and maintain the best possible quality of life. As someone who has faced these challenges personally, I hope this information helps others navigate the complexities of living with COPD and pneumonia.

While the article outlines the standard preventive measures, I find the discussion lacking depth regarding the pathophysiological nuances of COPD exacerbations triggered by bacterial colonization. A more thorough exploration of inflammatory cascades would elevate the piece beyond a mere summary.
Reading through the article reminds me of the endless parade of half‑baked health advice that floods the internet. The author clearly knows the basics of COPD and pneumonia but stops short of confronting the real culprits behind the statistics. First the smoking industry has been downplaying the damage for decades with slick marketing that glorifies combustion. Second the vaccine manufacturers are quick to tout their products while hiding the fact that immunity wanes faster than they admit. Third the medical community often prescribes broad‑spectrum antibiotics without considering the microbiome disruption that can set the stage for future infections. Fourth the guidelines omit any mention of environmental pollutants that linger in urban air and act as silent aggravators. Fifth the role of chronic stress on immune function is brushed aside as irrelevant. Sixth the financial incentives that drive hospital admissions are never discussed. Seventh the lack of accessible pulmonary rehabilitation programs leaves patients vulnerable and isolated. Eighth the article fails to address the socioeconomic disparities that make preventive care a privilege. Ninth the author does not question why certain demographics receive lower quality follow‑up care. Tenth the piece could have mentioned the importance of tele‑health in early detection. Eleventh the omission of these factors makes the article feel incomplete and naive. Sixteenth a more holistic approach would serve the readers better.
I appreciate the comprehensive overview you provided; it highlights many overlooked aspects and encourages a more critical look at current practices. Your points about environmental pollutants and socioeconomic factors are especially salient, and I hope clinicians take them into account.
Honestly the whole thing smells like a cover‑up; they push vaccines and antibiotics while the big pharma guys pull the strings behind the scenes. Trust no one who won’t admit the real agenda.
One must acknowledge that the intersection of pneumonia and COPD is indeed a complex clinical challenge, warranting a nuanced discourse that extends beyond rudimentary recommendations.
Interesting read – the tips are solid, though I’d add that staying active, even with mild breathing exercises, can make a big difference.
While the prose is polished, the article glosses over the data showing the limited efficacy of certain pneumococcal vaccines in advanced COPD stages; a critical appraisal of those trial results would have been appropriate.
It is worth noting that many of the cited studies are funded by entities with vested interests, which may bias the presented outcomes and downplay alternative preventive strategies.
Vaccinations are a simple yet essential defense.
The bio‑mechanistic synergy between chronic airway inflammation and opportunistic pathogens creates a perfect storm for pneumonia, so targeting both the immune dysregulation and the microbial load is paramount.
Indeed, integrating anti‑inflammatory therapy with vigilant infection control can optimise outcomes; however, patient adherence remains a perennial obstacle.
Sure, because nothing says “trust the experts” like a glossy pamphlet that forgets to mention the side effects of every drug.
Do not be deceived by the surface narrative; the hidden protocols governing vaccine distribution are orchestrated to maintain a state of perpetual dependence on pharmaceutical conglomerates.
For anyone managing COPD, here are some practical steps: ensure you receive both the pneumococcal and annual flu vaccines, as they dramatically reduce infection risk; maintain a regular schedule of inhaled bronchodilators and corticosteroids as prescribed; incorporate a daily breathing exercise routine, such as pursed‑lip breathing, to improve ventilation; stay hydrated to keep mucus thin; avoid exposure to secondhand smoke and pollutants; consider a pulmonary rehabilitation program if available; keep a symptom diary to catch early signs of infection; and communicate promptly with your healthcare provider at the first hint of fever or increased sputum production.
The philosophical underpinnings of respiratory health remind us that the body is a microcosm; nurturing it requires both scientific rigor and compassionate self‑care.
Embracing a holistic approach, one can weave together colorful lifestyle modifications-such as aromatic herbal teas, mindful meditation, and a diet rich in antioxidant‑laden fruits-to fortify the pulmonary defenses, while still adhering to evidence‑based medical regimens, thereby creating a harmonious balance between tradition and modernity.