Endometriosis Fertility Preservation Calculator
Calculate Your Success Rate
Estimated Success Rate for Pregnancy (Live Birth)
Understanding Your Results
Success rates are highest for women under 35 with mild endometriosis who choose egg freezing. For women over 38, success rates decline significantly.
Key factors affecting your results:
- Age: Fertility preservation success rates decline after age 35
- Endometriosis stage: More advanced disease may affect ovarian reserve
- Method choice: Embryo freezing generally has higher success rates than egg freezing
Next steps: Consult a reproductive endocrinologist to discuss personalized options based on your AMH levels, ovarian follicle count, and medical history.
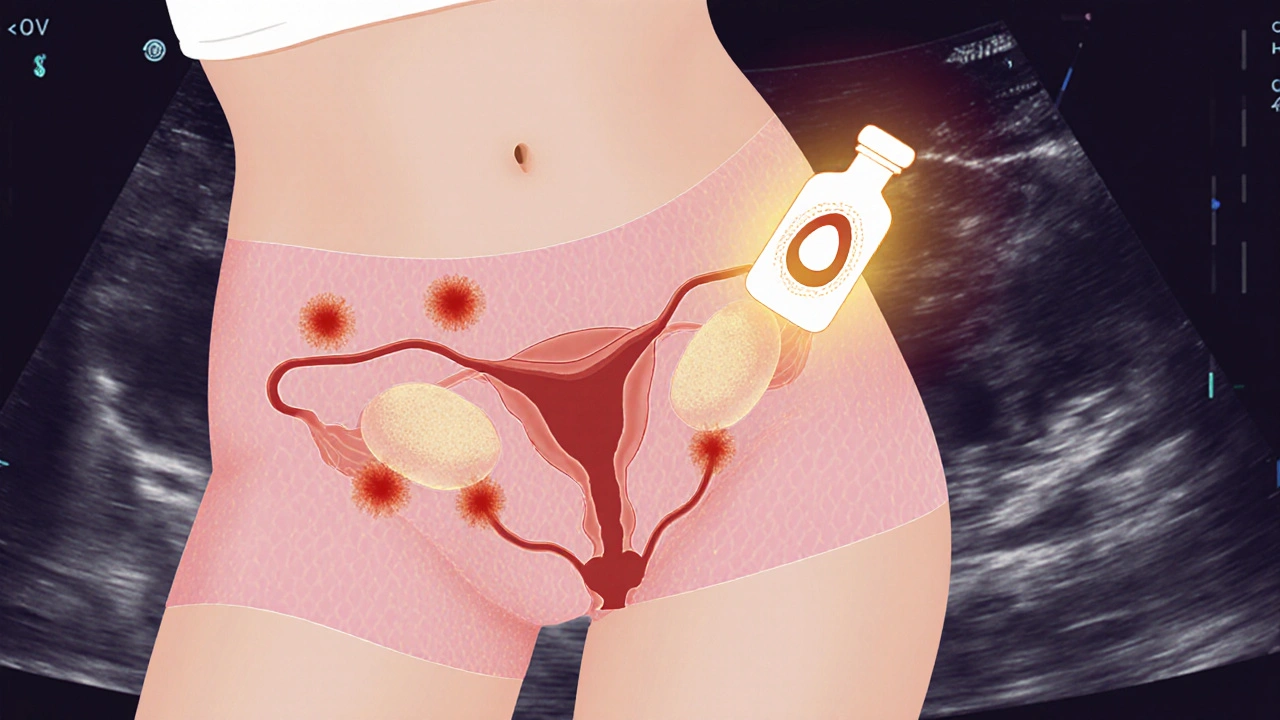
Women diagnosed with Endometriosis is a chronic condition where tissue similar to the uterine lining grows outside the uterus, often on the ovaries, fallopian tubes, or pelvic lining. This tissue can cause pain, inflammation, and scar tissue that may impair fertility. Understanding how fertility preservation works gives you a proactive path forward, especially if you’re planning to delay pregnancy or face surgical treatment.
Quick Takeaways
- Endometriosis can reduce egg quality and ovarian reserve, but many women still conceive naturally.
- Preservation methods include egg freezing, embryo freezing, and ovarian tissue cryopreservation.
- Timing is crucial -‑ the earlier you act, the higher the success rates.
- Consult a reproductive endocrinologist to tailor a plan based on disease stage, age, and personal goals.
- Consider surgical options like laparoscopic excision to improve natural fertility before opting for preservation.
How Endometriosis Affects Fertility
Research from the American Society for Reproductive Medicine shows that up to 30‑40% of women with endometriosis experience infertility. The main mechanisms are:
- Distorted pelvic anatomy causing blocked fallopian tubes.
- Inflammatory environment lowering egg quality.
- Reduced ovarian reserve measured by AMH test (Anti‑Müllerian Hormone levels).
Even mild disease (Stage I‑II) can affect the ovarian reserve, so early assessment matters.
When to Consider Fertility Preservation
Key moments to start the conversation:
- Diagnosis of moderate‑to‑severe endometriosis (Stage III‑IV).
- Before undergoing laparoscopic or robotic excision of ovarian endometriomas.
- If you plan to start hormone‑suppressive therapy (e.g., GnRH agonists) that may delay ovulation for months.
- When age is approaching the mid‑30s, as ovarian reserve declines faster with endometriosis.
Discussing options with a reproductive endocrinologist helps align medical timing with your family‑building timeline.
Preservation Options Explained
Below is a side‑by‑side look at the three main techniques used for women with endometriosis.
| Method | Procedure | Typical Success Rate (Live Birth) | Cost (US$) | Pros | Cons |
|---|---|---|---|---|---|
| Egg Freezing | Hormonal stimulation → egg retrieval → vitrification | 30‑40% (if frozen before age 35) | 8,000‑12,000 per cycle | Preserves own genetic material; no partner needed now | Requires ovarian stimulation; may worsen endometriosis symptoms |
| Embryo Freezing | Egg retrieval + fertilization with sperm → embryo vitrification | 35‑45% (if frozen before age 35) | 10,000‑15,000 per cycle | Higher implantation rates; can use donor sperm later | Requires sperm at time of retrieval; ethical considerations for unused embryos |
| Ovarian Tissue Cryopreservation | Laparoscopic removal of ovarian cortex → tissue freezing | ~20% (still experimental for endometriosis) | 6,000‑9,000 (plus surgery) | Option for pre‑pubescent girls or women who cannot undergo stimulation | Requires future re‑implantation surgery; lower success data |

Step‑by‑Step Guide to Egg Freezing (Most Common Choice)
- Initial consultation with a reproductive endocrinologist to assess ovarian reserve (AMH, antral follicle count) and discuss disease stage.
- Baseline ultrasound to map endometriomas and decide if surgical removal is needed first.
- If surgery is advised, schedule laparoscopic excision of endometriomas. Recovery typically 2‑4 weeks.
- After healing, begin controlled ovarian hyperstimulation (COH) -‑ daily injections of FSH or hMG for 10‑12 days.
- Monitor follicles via ultrasound and hormone levels; trigger final maturation with hCG when follicles reach 18‑20mm.
- Egg retrieval performed under mild sedation; 30‑40minutes to collect mature oocytes.
- Immediately vitrify (flash‑freeze) each egg using a closed‑system device to avoid contamination.
- Store eggs in a certified cryobank; most clinics offer a 10‑year guarantee with options for extension.
Key tip: If you have large endometriomas (>3cm), removing them before stimulation can improve egg yield and reduce risk of fluid leakage during retrieval.
Alternative Path: Ovarian Tissue Cryopreservation
This method is gaining attention for women who cannot take hormonal meds because of severe pain or hormone‑sensitive disease. A small piece of ovarian cortex is removed laparoscopically, sliced into thin strips, and frozen. When you’re ready for pregnancy, the tissue is thawed and transplanted back, often restoring natural ovulation.
Success stories are emerging, particularly in Europe, but the technique remains considered experimental in the U.S. Discuss eligibility and potential trial enrollment with your reproductive specialist.
Integrating Surgical Management with Preservation
Many clinicians recommend a two‑step approach: first, surgical removal of endometriotic lesions to improve pelvic anatomy and reduce inflammation, followed by preservation. Studies in 2023 showed that women who had laparoscopic excision before egg freezing had a 12% higher average oocyte count compared to those who froze without surgery.
However, surgery itself can temporarily lower ovarian reserve, especially if cystectomy involves stripping ovarian tissue. Your surgeon should aim for a “cortical strip” technique that spares as much healthy ovarian cortex as possible.
Cost, Insurance, and Financial Planning
Insurance coverage for fertility preservation varies by state. California mandates that insurers cover egg freezing for medical indications like cancer; endometriosis qualifies under many plans as a “medical condition affecting fertility.” Check with your provider and request a pre‑authorization letter.
Many clinics offer financing plans: $200‑$300 per month over 24‑36 months. Some employers include fertility benefits as part of health‑wellness perks. If cost is a barrier, look into nonprofit grants such as the RESOLVE Endometriosis Foundation scholarship program.
Emotional and Psychological Support
Facing chronic pain and uncertain fertility can be overwhelming. Connecting with support groups-both online (e.g., Endometriosis Foundation of America forums) and local (San Diego Endometriosis Support Circle)-provides shared experiences and coping strategies. A mental health professional familiar with reproductive concerns can help manage anxiety and decision‑making stress.
Putting It All Together: Decision Checklist
- Confirm endometriosis stage and ovarian reserve (AMH, AFC).
- Identify your timeline: do you want children now, later, or are you unsure?
- Discuss surgical options: will removing endometriomas improve natural fertility?
- Choose preservation method based on age, ovarian reserve, and personal values.
- Verify insurance coverage and explore financing if needed.
- Plan follow‑up appointments: post‑surgery healing, hormone monitoring, and embryo/egg storage logistics.
- Seek emotional support and keep a journal of symptoms, appointments, and feelings.
Following this checklist helps you stay organized and reduces the chance of missing critical steps.
Next Steps After Freezing
Once your eggs or tissue are stored, you still need a plan for eventual use:
- When you decide to conceive, schedule a thaw cycle with your clinic.
- Consider in‑vitro fertilization (IVF) using your thawed eggs. Success rates mirror fresh IVF if thawing is done within 5‑7 years.
- If you have a partner now, use his sperm; if not, you can opt for donor sperm at the time of fertilization.
- Keep your cryobank informed about storage duration and any policy changes.
Remember, you can still attempt natural conception before using frozen material-many women conceive naturally after surgery even if they previously froze eggs.
Frequently Asked Questions
Can endometriosis be cured?
There is no permanent cure, but surgical removal of lesions and hormonal therapy can control pain and improve fertility. Ongoing research aims to develop targeted medical treatments.
Is egg freezing safe for women with endometriomas?
Yes, but doctors often recommend removing large endometriomas first to lower the risk of fluid leakage during retrieval and to increase the number of healthy eggs collected.
How long can frozen eggs be stored?
Studies show that eggs remain viable for at least 10‑15 years. Most clinics offer indefinite storage as long as fees are paid.
Do insurance plans cover ovarian tissue cryopreservation?
Coverage is less common than for egg freezing. Some plans cover it under experimental procedures or as part of a cancer‑related fertility preservation benefit. Always verify with your insurer.
What are the emotional challenges of fertility preservation?
Feelings of loss, anxiety about future outcomes, and financial stress are common. Joining support groups, seeing a therapist familiar with reproductive health, and maintaining open communication with partners can help manage these emotions.

Regarding ovarian reserve, an AMH panel and antral follicle count give the clearest picture before deciding on any preservation method.
Oh sure, because a single blood test magically solves the whole hormonal roller‑coaster of endometriosis.
The intersection of endometriosis severity and reproductive timing creates a uniquely challenging clinical scenario that demands both scientific rigor and compassionate counseling.
While the calculator presented in the post offers a helpful heuristic, it inevitably reduces a multidimensional decision to a few numerical inputs, which can be misleading if not contextualized.
First, the pathological burden of endometriosis, especially in stages III and IV, often correlates with inflammatory mediators that compromise oocyte quality beyond what age alone predicts.
Second, the variability of ovarian reserve among patients with similar AMH levels is considerable, owing to factors such as prior cystectomy, genetic predisposition, and even lifestyle influences like smoking.
Third, the choice between egg and embryo cryopreservation should reflect personal circumstances, including the presence of a partner, future plans for donor gametes, and ethical comfort with storing embryos.
Fourth, ovarian tissue cryopreservation, while experimental, provides a vital option for those who cannot tolerate hormonal stimulation, yet the success rates remain modest and the procedure requires specialized surgical expertise.
Fifth, a multidisciplinary approach that integrates a reproductive endocrinologist, a skilled minimally invasive surgeon, and a mental health professional has been shown to improve both objective outcomes and patient satisfaction.
Sixth, recent evidence suggests that performing laparoscopic excision of endometriomas prior to controlled ovarian stimulation can increase the number of mature oocytes retrieved, though the trade‑off may be a transient dip in the ovarian reserve.
Seventh, insurance coverage for fertility preservation is heterogeneous across states, and patients should proactively request pre‑authorization letters to avoid unforeseen financial burden.
Eighth, emerging data from health economics analyses indicate that early preservation before the age of 35 can be cost‑effective when considering the cumulative probability of live birth over a decade.
Ninth, patients should be encouraged to keep a detailed log of symptom patterns, medication cycles, and hormonal assay results, as this longitudinal data can inform more precise timing of stimulation protocols.
Tenth, the psychological impact of a chronic disease combined with fertility uncertainty cannot be overstated; support groups and counseling can mitigate anxiety that might otherwise affect treatment adherence.
Eleventh, while the calculator’s success percentages are grounded in population averages, individual outcomes can deviate substantially, especially for those with atypical ovarian reserve metrics.
Twelfth, clinicians ought to present the data as a range rather than a point estimate, emphasizing that live‑birth rates are influenced by embryo quality, uterine receptivity, and laboratory proficiency.
Finally, the decision matrix should be revisited annually, because disease progression, age, and personal goals evolve, and what may have been an optimal strategy at 28 could differ markedly at 37.
Look, the “multidisciplinary approach” you glorify sounds like a buzzword buffet-do we really need a circus of specialists to decide whether to freeze some eggs? Also, your claim about cost‑effectiveness ignores the out‑of‑pocket nightmare many patients face, especially when insurance decides to play hide‑and‑seek.
In the grand scheme, juggling hormones feels like a metaphor for the endless politics of our own borders.
It might seem overwhelming, but breaking the process into small steps-first test, then consult, then decide-can make it feel manageable.
Honestly, the biggest hurdle isn’t the science; it’s finding a clinic that treats endometriosis patients with the same respect you’d give anyone else trying to build a family.
Totally get you! 👍 Finding that supportive team makes all the difference. 😊
From an evidence‑based standpoint, the ethical justification for preserving gametes in cases where disease pathology already compromises embryo viability remains tenuous and warrants stricter regulatory oversight.
While regulations matter, we must also remember the human stories behind the data-each frozen egg represents hope, resilience, and a future that many women refuse to surrender.
It could be argued that the emphasis on technological interventions diverts attention from preventive strategies that might reduce the incidence of endometriosis‑related infertility altogether.