
Steroid Pre-Medication Dosing Calculator
Steroid Pre-Medication Calculator
Note: This calculator is for reference only. Always follow your medical team's specific instructions.
Why Pre-Medication Matters in Modern Medicine
Every year, millions of patients get contrast dye for CT scans, undergo chemotherapy, or enter surgery. For many, these procedures are routine. But for some, they trigger dangerous reactions-nausea so severe it leads to dehydration, rashes that swell the face, or even breathing trouble. These aren’t rare accidents. They’re predictable risks-and they can be prevented. Pre-medication isn’t about giving everyone extra drugs. It’s about giving the right drugs to the right people at the right time. The goal? Stop reactions before they start. And the evidence shows it works. Hospitals that use standardized pre-medication protocols cut moderate to severe contrast reactions from nearly 1 in 200 patients down to less than 1 in 2,500. The three main tools? Antiemetics to stop vomiting, antihistamines to block allergic responses, and steroids to calm the immune system. Used together, they form a shield. But only if they’re used correctly.When and Why Steroids Are Used
Steroids like prednisone and methylprednisolone don’t work like painkillers. They don’t give instant relief. They work slowly-by quieting down the body’s overactive immune response hours before a procedure. That’s why timing matters more than the dose. For outpatient scans, Yale’s protocol calls for 50mg of oral prednisone taken 13, 7, and 1 hour before contrast injection. That’s not a suggestion-it’s a requirement. If you give it too late, the steroid won’t have time to build up in the system. A patient scheduled for a same-day CT scan at 10 a.m. needs to start the first dose by 9 p.m. the night before. That’s a big ask for someone who just got called in for an urgent scan. In emergency rooms and hospitals, where there’s no time for oral meds, IV methylprednisolone (40mg) given 4 hours before the procedure is the standard. Hydrocortisone (200mg IV) is the backup if methylprednisolone isn’t available. These IV options work faster because they bypass the digestive system. Pediatric dosing is weight-based: 0.7mg per kg of body weight, capped at 50mg. A 20-pound toddler gets about 6mg, not a full adult dose. Giving kids adult doses isn’t just wrong-it’s dangerous. The catch? Steroids don’t prevent all reactions. They reduce moderate ones by about 96%, but only cut severe reactions by 75%. And they don’t help with nausea. That’s why they’re never used alone.Antihistamines: First-Gen vs. Second-Gen
Antihistamines block histamine, the chemical that causes itching, hives, and swelling during allergic reactions. But not all antihistamines are created equal. First-generation drugs like diphenhydramine (Benadryl®) work fast. But they make you sleepy-up to 43% of patients report drowsiness. In a radiology suite, that’s a problem. A drowsy patient can’t follow breathing instructions. They might move during the scan. That means repeat images, more radiation, and longer wait times. Second-generation antihistamines like cetirizine (Zyrtec®) are better. They’re just as effective at preventing reactions, but cause drowsiness in only 15% of people. That’s why most hospitals now prefer cetirizine for outpatients. The dose? 10mg, taken within an hour before the procedure. For kids under 6 months, diphenhydramine is still used-1mg per kg, max 50mg-because cetirizine isn’t approved for such young infants. For older kids, cetirizine is dosed by age: 2.5mg for ages 6 months to 2 years, 5mg for ages 2 to 6, and 10mg for 6 and up. One thing to watch: antihistamines alone don’t stop anaphylaxis. They’re part of a team. Steroids handle the deeper immune response. Antihistamines handle the surface symptoms. Together, they cover more ground.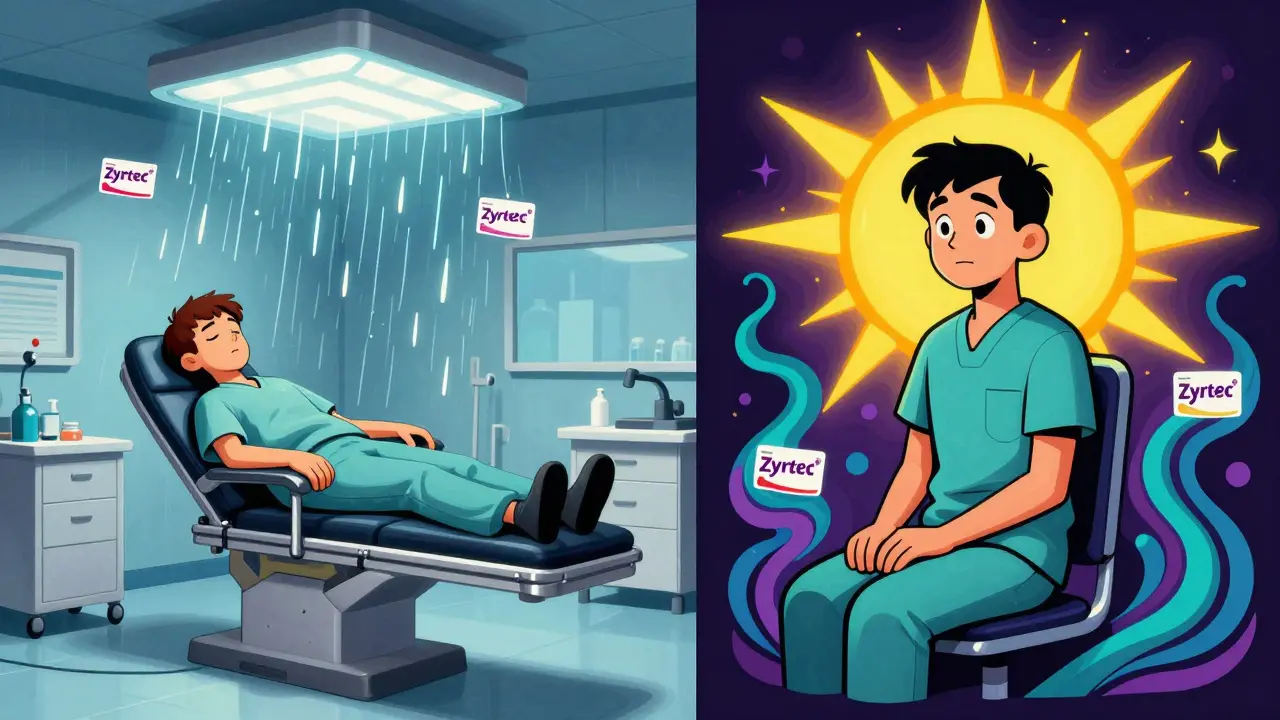
Antiemetics: The Game-Changer for Chemotherapy Patients
If you’ve ever thrown up after chemo, you know it’s not just unpleasant-it’s debilitating. That’s why antiemetics are now standard before treatment. Old-school protocols used just one drug-ondansetron, for example. Today, the gold standard is triple therapy: a 5-HT3 antagonist (like ondansetron), an NK1 antagonist (like aprepitant), and dexamethasone (a steroid). This combo works in three different ways to block nausea signals in the brain and gut. The numbers speak for themselves. With triple therapy, 70-80% of patients have zero vomiting in the first 24 hours. With just one or two drugs, that number drops to 40-50%. A 2023 meta-analysis showed triple therapy cut nausea rates from 56.7% to 28.4%. For high-risk chemo like cisplatin, this isn’t optional. It’s mandatory. But even with the best drugs, 15-20% of patients still get breakthrough nausea. That’s why nurses now ask: "Did you take your antiemetic on time?" and "Did you eat something light?" Small things matter. Newer drugs like fosnetupitant (a next-gen NK1 blocker) are on the horizon. They’re given as a single IV injection instead of pills, which helps patients who struggle with swallowing or keeping meds down. But for now, the triple combo remains the standard.Who Gets Pre-Medication-and Who Doesn’t
Not everyone needs it. Giving drugs to everyone just in case isn’t safer-it’s riskier. More drugs mean more side effects, more errors, and more cost. The rule is simple: pre-medicate only if you’ve had a prior reaction to contrast or chemo. If you’ve never reacted before, you’re not at high risk. Studies show that patients with no history of reactions have less than a 0.1% chance of having one-even without pre-medication. That’s why Yale and other top hospitals don’t pre-medicate first-time patients. They track who’s had reactions and flag them in the system. If a patient says, "I got sick after my last CT," the pharmacy gets an alert. The nurse double-checks. The doctor confirms. The big mistake? Overuse. Some clinics give steroids and antihistamines to every patient with "mild allergies"-like hay fever or a penicillin rash from 10 years ago. That’s not evidence-based. That’s fear-driven. And it’s wasteful.How Hospitals Get It Right (and Where They Fail)
The best hospitals don’t just have protocols. They build systems around them. At Johns Hopkins, they added barcode scanning to every pre-medication step. Before giving a dose, the nurse scans the patient’s wristband, the medication, and the time. If anything’s off-wrong drug, wrong dose, wrong time-the system stops them. Since 2022, their contrast reaction rate dropped 92%. But many hospitals still struggle. A 2022 survey found that 68% of hospitals had medication reconciliation errors with pre-med orders. Someone forgets to update the chart after a patient takes prednisone at home. The nurse gives it again in the hospital. Double dose. Risk of high blood sugar, mood swings, or infection. Shift changes are another weak point. A patient gets their first prednisone at 9 p.m. The night nurse gives it. The morning nurse doesn’t know. The patient misses the 7 a.m. dose. The scan goes ahead. Reaction happens. Solutions? Electronic health records with automated alerts. Standardized order sets. Pharmacy-led verification teams. Training that’s not a one-time webinar-but a monthly check-in. Yale spent six months getting their protocol right. They had meetings with radiology, pharmacy, nursing, and IT. They built alerts into the EHR. They trained everyone. After 12 months, 94.7% of staff followed the protocol every time.
What You Can Do as a Patient
If you’re scheduled for a scan or chemo:- Ask: "Do I need pre-medication? Why?" If you’ve never had a reaction, you probably don’t.
- If you’re told to take prednisone: mark your calendar. Set three alarms. Write down the times: 13, 7, and 1 hour before.
- For antihistamines: ask for cetirizine (Zyrtec®) instead of Benadryl®. You’ll feel better afterward.
- For chemo: ask if you’re getting the triple therapy. If not, ask why.
- Bring a list of all your meds-including vitamins and supplements. Many pre-med drugs interact with other pills.
- If you feel dizzy, itchy, or nauseated during the procedure-speak up. Don’t wait. The staff can stop and treat it.
What’s Next for Pre-Medication?
The future isn’t about more drugs. It’s about smarter predictions. A 2023 study used machine learning to analyze 12,000 patient records. The algorithm looked at age, gender, history of asthma, prior reactions, even lab values-and predicted contrast reactions with 83.7% accuracy. That’s better than most doctors guess. Soon, your EHR might auto-flag you as high-risk based on your history-not your doctor’s memory. That means fewer people get unnecessary drugs. And more high-risk patients get the protection they need. The American Society of Clinical Oncology says triple therapy isn’t going away. It’s getting refined. New drugs are coming. But the core idea stays the same: prevent reactions with the right drugs, at the right time, for the right people.FAQ
Do I need pre-medication for a CT scan if I’ve never had a reaction before?
No, you don’t. Pre-medication is only recommended for patients who’ve had a prior hypersensitivity reaction to contrast dye. Studies show that first-time patients have less than a 0.1% risk of a reaction. Giving steroids and antihistamines to everyone increases side effects and medication errors without improving safety.
Can I take my antiemetic pills the night before chemo?
It depends on the drug. Some, like aprepitant, are designed to be taken the night before and again the next morning. Others, like ondansetron, are best taken 30-60 minutes before chemo. Always follow your oncology team’s exact timing instructions. Taking them too early can reduce their effectiveness.
Why do I need to take prednisone three times before a scan?
Steroids like prednisone work by suppressing immune activity over time. A single dose doesn’t build up enough in your system to block a reaction. Taking 50mg at 13, 7, and 1 hour before the scan ensures steady, rising levels in your blood when the contrast is injected. Skipping doses reduces protection by up to 60%.
Is cetirizine better than Benadryl for pre-medication?
Yes, for most adults. Cetirizine (Zyrtec®) is just as effective at preventing allergic reactions but causes far less drowsiness-only 15% of users report sleepiness compared to 43% with Benadryl. Less drowsiness means fewer falls, better scan cooperation, and faster recovery. Most hospitals now prefer cetirizine unless the patient is under 6 months old.
What if I miss a dose of my pre-medication?
Call your provider immediately. If you miss the 13-hour prednisone dose, you might still get the 7-hour and 1-hour doses, but protection drops significantly. For IV steroids in the hospital, the team may delay the scan or give a higher IV dose. Never assume you’re still protected. Always inform your care team.


Just took Zyrtec before my CT and skipped the steroids-never had a reaction before. Felt fine. Why give people a whole pharmacy if they don’t need it?
Yeah but what if you’re one of those people who ‘never had a reaction’… until you do? And then it’s like, oh wait, I should’ve taken the prednisone? I’m not saying everyone needs it-but I’m not convinced the 0.1% risk is worth ignoring either.
Okay, but like… why do we even have protocols if we’re just gonna… *shrug* and let people decide? I mean, if the hospital’s got the system, why not use it? I’ve seen people miss their 7am dose because they thought ‘it’s just one pill’… and then they turn purple. Not cute. Not cute at all.
As someone who’s been through chemo and had to take 5 different pills before every session-yes, the triple therapy saved my life. I cried when I realized I wasn’t gonna throw up for 24 hours straight. But also? Please don’t make patients feel guilty for asking questions. We’re scared. We’re tired. We just want to know we’re being treated like humans, not numbers. Thank you for writing this. Truly.
It is imperative to note that the implementation of standardized, evidence-based pre-medication protocols has demonstrably reduced adverse event rates by over 90% in institutions that prioritize systematic integration-via electronic alerts, pharmacy verification, and staff education. Deviations from protocol, even well-intentioned ones, introduce systemic risk. The data is unequivocal.
Let’s be real-most of these protocols exist because lawyers told hospitals to do it, not because doctors actually believe in them. I’ve worked in three ERs. Half the nurses don’t even know what ‘methylprednisolone’ is. And you think giving steroids to every person with ‘mild allergies’ is safe? Please. You’re just creating more side effects for people who don’t need them. It’s medical theater.
Interesting how the US focuses so much on pre-medication, but in Nigeria, we rarely use steroids for contrast unless it’s a known history. We rely more on observation and immediate response protocols. Maybe the real issue isn’t just the drugs-it’s how we define risk? I’ve seen patients react even after full pre-med. And others who got nothing and walked away fine.
My cousin took Benadryl before her scan and passed out in the waiting room. They had to call a code. Zyrtec’s the way to go. No sleepiness, same protection. Why are we still giving people the old stuff? Just… stop.