Egg Freezing: A Practical Guide to Preserving Your Fertility
When working with egg freezing, the process of cooling a woman's eggs for future use. Also known as oocyte cryopreservation, it offers a way to pause the biological clock and keep reproductive options open. This technique falls under the broader field of fertility preservation, strategies that safeguard a person's ability to have children later in life. By storing eggs now, you can plan family building on your own timeline, whether you’re dealing with a medical condition, career plans, or simply want flexibility.
How the Process Connects to Hormones, Stimulation, and Cryopreservation
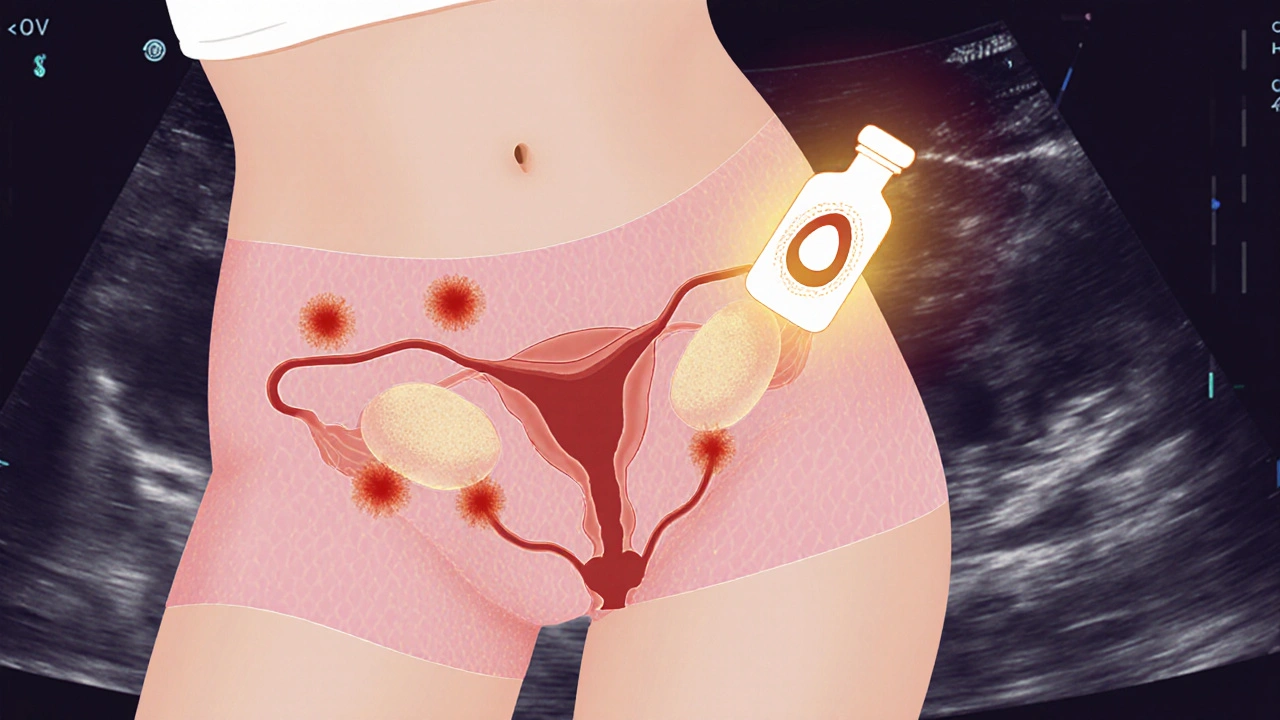
The first step in egg freezing is ovarian stimulation, which uses injectable hormones to encourage the ovaries to produce multiple mature eggs. This stage is essential because it increases the number of eggs you can freeze, boosting the chance of a successful pregnancy later. Once the eggs reach the right maturity, they are retrieved in a short outpatient procedure. The retrieved eggs are then subjected to cryopreservation, a controlled cooling method that prevents ice crystal formation and keeps cells viable for years. Vitrification, a fast‑freezing technique, has become the gold standard, offering survival rates above 90% after thawing.
Egg freezing doesn’t happen in isolation. It directly supports in‑vitro fertilization (IVF), where frozen eggs are later thawed, fertilized with sperm, and transferred to the uterus. In many cases, couples or solo patients use frozen eggs to bypass age‑related declines in egg quality, making IVF outcomes more predictable. This relationship creates a clear semantic chain: egg freezing enables cryopreservation, which fuels IVF success, and both belong to the fertility preservation umbrella.
Cost is another practical factor. Prices vary by clinic, geographic region, and the number of cycles needed to achieve a target egg count. Many insurers start covering at least part of the process for patients undergoing medical treatments that threaten fertility, such as chemotherapy. Understanding insurance policies, payment plans, and potential hidden fees helps you budget effectively and avoid surprises.
Legal and ethical considerations also shape the egg freezing landscape. Different countries have distinct regulations on how long eggs can be stored, who may access them, and what happens to unused eggs after a certain period. Knowing your local laws ensures you respect consent requirements and make informed decisions about long‑term storage agreements.
Beyond the medical side, emotional support plays a big role. The hormonal injections can cause mood swings, and the waiting period before a future pregnancy can be stressful. Counseling, support groups, and reliable information sources help manage expectations and keep the experience positive. When you combine medical facts with realistic emotional guidance, egg freezing becomes a well‑rounded option rather than a vague hope.
Below you’ll find a collection of articles that dig deeper into each of these topics – from hormonal protocols and cost breakdowns to legal frameworks and personal stories of people who chose egg freezing. Use them to build a clear picture of what the process looks like, what you might expect, and how to make the best choices for your future family plans.
Learn how endometriosis impacts fertility and explore preservation options like egg freezing, embryo banking, and ovarian tissue cryopreservation with practical steps and considerations.