Endometriosis: Understanding, Managing, and Living With It
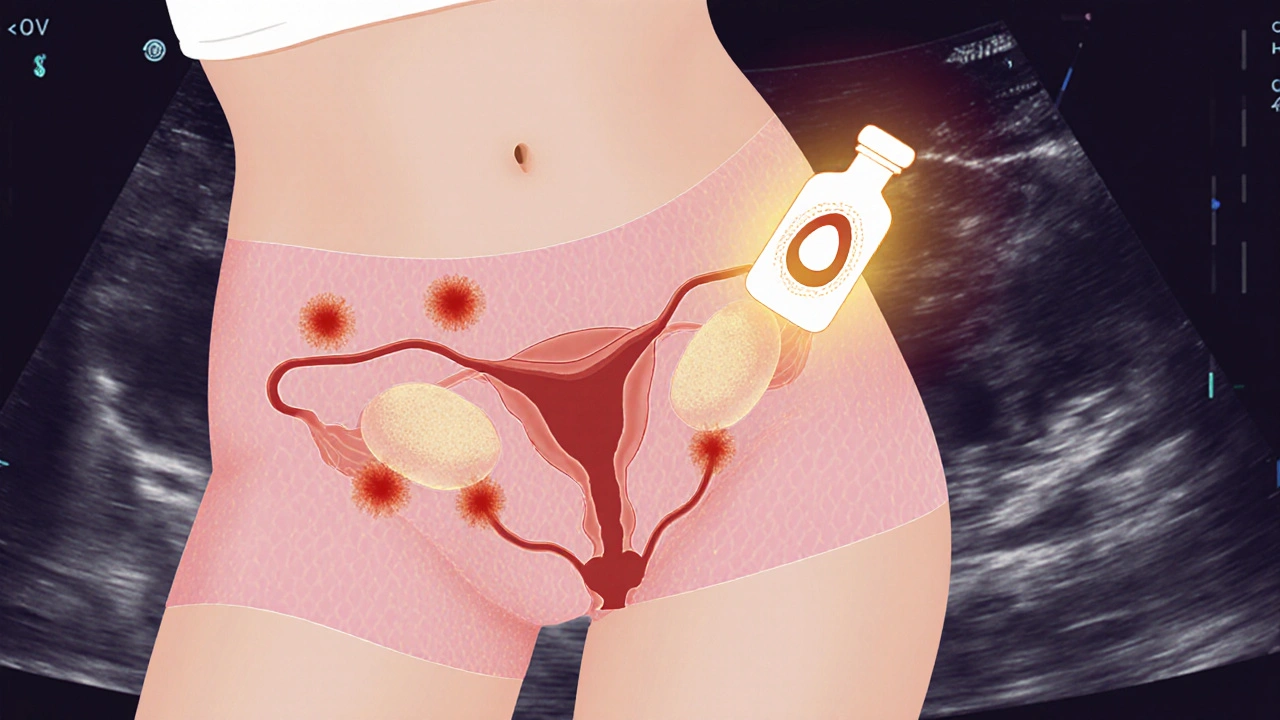
When dealing with Endometriosis, a chronic condition where tissue similar to the uterine lining grows outside the uterus, causing pain and fertility issues. Also known as pelvic endometriosis, it commonly affects women of reproductive age and can impact daily life. This page gives you a clear picture of what the condition means and why it matters.
One of the main ways doctors tackle the disease is through Hormonal Therapy, medications that adjust estrogen levels to slow or stop ectopic tissue growth. Hormonal therapy includes oral contraceptives, progestins, and GnRH agonists. It often reduces pelvic pain and improves chances of conceiving, making it a cornerstone of endometriosis care.
When medication alone isn’t enough, many turn to Laparoscopic Surgery, a minimally invasive procedure that removes or destroys endometrial implants. Surgeons can also excise deep infiltrating lesions, which helps restore normal anatomy and may boost fertility. The decision to operate depends on pain severity, lesion location, and personal goals.
Pain management often starts with NSAIDs, non‑steroidal anti‑inflammatory drugs that lower prostaglandin production and ease menstrual cramps. Ibuprofen or naproxen taken during the first few days of bleeding can provide quick relief, but they don’t treat the underlying tissue growth.
How Diagnosis Connects to Treatment Choices
Diagnosing endometriosis usually involves a combination of symptom review, pelvic exam, and imaging such as transvaginal ultrasound or MRI. Definitive proof comes from laparoscopic visualization and biopsy, which also offers an opportunity to start surgical treatment immediately. Early detection shortens the time to effective therapy, whether hormonal or surgical.
Beyond the clinical side, lifestyle tweaks play a supportive role. Regular exercise can lower estrogen levels, while a diet rich in omega‑3 fatty acids and low in processed foods may reduce inflammation. Stress management techniques—like yoga or mindfulness—help keep hormone swings in check, indirectly easing pain.
Fertility is a frequent concern for women with endometriosis. In cases where ovarian reserve is compromised, assisted reproductive technologies such as IVF become viable options. Combining hormonal suppression before IVF cycles can improve egg quality and implantation rates.
Each treatment path carries its own set of trade‑offs. Hormonal therapy may cause mood changes or bone density loss if used long‑term. Surgery carries risks of scar tissue and recurrence, as endometriosis can regrow. Understanding these nuances helps patients weigh benefits against possible side effects.
The collection of articles below dives deeper into these topics. You’ll find practical guides on medication comparisons, safety tips for specific drugs, and evidence‑based strategies for managing chronic pelvic pain. Whether you’re looking for the latest on hormonal options or surgical advances, the resources are organized to give you actionable insight.
Take a look at the posts ahead to see detailed breakdowns of drug choices, real‑world treatment experiences, and expert advice that can empower you to make informed decisions about your health.
Learn how endometriosis impacts fertility and explore preservation options like egg freezing, embryo banking, and ovarian tissue cryopreservation with practical steps and considerations.