When you’re 70, your body doesn’t process medicine the same way it did at 30. That’s not just a myth-it’s science. The liver and kidneys, two of your body’s main drug-processing organs, change as you age. These changes can turn a safe dose into a dangerous one. For older adults, taking the same pills they did decades ago can lead to dizziness, falls, confusion, or even hospitalization. And it’s happening more than you think: 10% of hospital admissions in seniors are caused by bad reactions to medications.
What Happens to the Liver as You Age?
Your liver shrinks. By the time you hit 80, it’s lost about 30% of its mass. Blood flow through it drops by nearly 40%. That means drugs move through your liver slower. If your liver can’t process a drug quickly, it builds up in your blood. That’s why a standard dose of a painkiller or antidepressant might hit an older person like a sledgehammer.
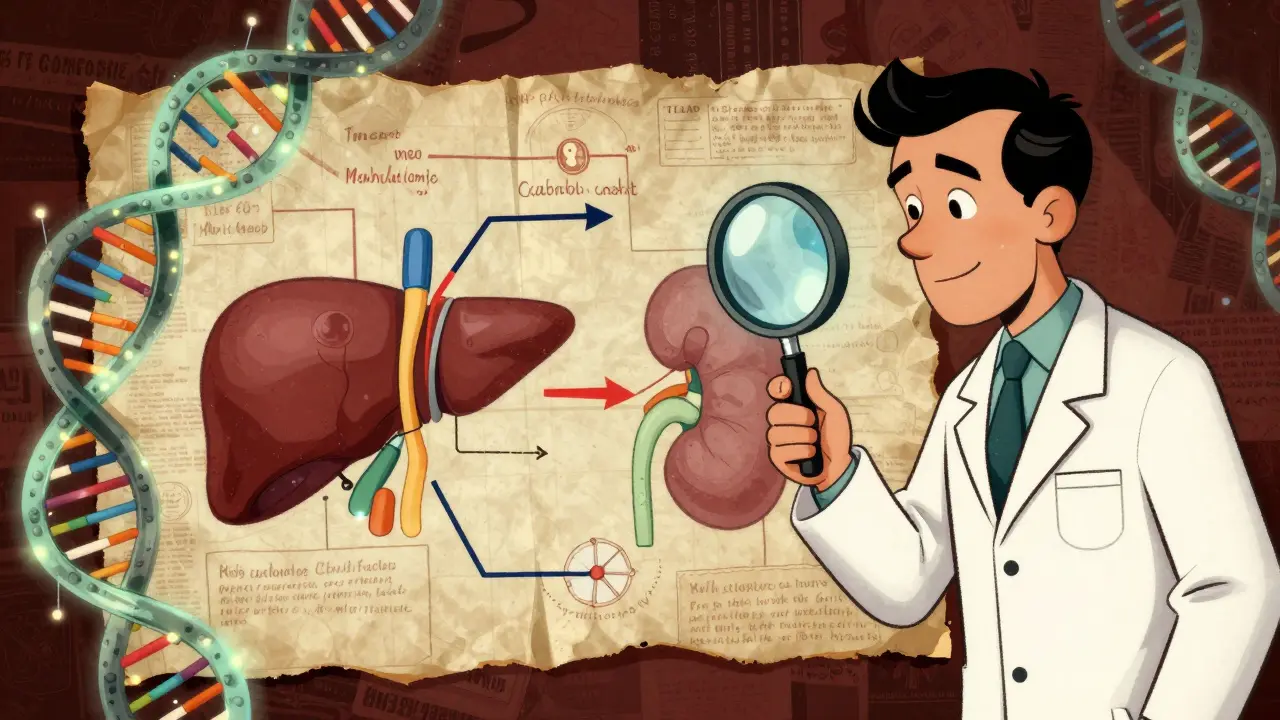
Not all drugs are affected the same way. Some are “flow-limited”-meaning their clearance depends mostly on how much blood flows through the liver. Propranolol, lidocaine, and morphine fall into this group. With less blood flow, their clearance drops by about 40%. That’s a huge change. Other drugs are “capacity-limited”-they depend more on enzyme activity. Diazepam, phenytoin, and theophylline are examples. Their metabolism doesn’t drop as much because the enzymes that break them down stay mostly intact.
Here’s the tricky part: some medications need to be activated by the liver to work. These are called prodrugs. Perindopril, an ACE inhibitor used for blood pressure, is one. If your liver is slower, the drug doesn’t convert properly. You might think it’s not working, but the problem isn’t the dose-it’s your liver.
First-pass metabolism also weakens. That’s the process where the liver breaks down a drug before it even enters your bloodstream. When this slows down, more of the drug gets through. For drugs like verapamil or propranolol, that means bioavailability can jump by 25-50%. A pill that used to give you a gentle effect now floods your system.
How Kidney Changes Impact Medications
Your kidneys filter waste-and drugs-from your blood. As you age, your glomerular filtration rate (GFR) drops by 30-50% between ages 30 and 80. That’s not a small dip. It’s a major slowdown. Many drugs, like antibiotics, diuretics, and pain relievers, are cleared almost entirely by the kidneys. If your kidneys aren’t filtering well, those drugs stick around longer. That increases the risk of toxicity.
Here’s where it gets confusing: your serum creatinine-a common blood test used to check kidney function-often stays normal even when your kidneys are failing. Why? Because older adults lose muscle mass. Less muscle means less creatinine is made. So the test looks fine, but your kidneys aren’t working well. That’s why doctors can’t rely on creatinine alone. They need to calculate your estimated GFR using formulas like CKD-EPI or Cockcroft-Gault.
Some drugs are especially dangerous if your kidneys are weak. Digoxin, lithium, and metformin are classic examples. A standard dose of metformin can cause lactic acidosis in someone with reduced kidney function. That’s why many guidelines now say: start low, go slow, and monitor kidney function every few months if you’re on these drugs.
And here’s a newer discovery: when kidneys fail, liver enzymes can drop too. Studies show that kidney impairment can reduce CYP450 enzyme activity by up to 20%. That means even drugs processed by the liver might build up if your kidneys are struggling. It’s a double hit.
Why Some Drugs Are Riskier Than Others
Not all medications are created equal in older adults. Some are outright dangerous. The Beers Criteria®-a widely used list of potentially inappropriate medications for seniors-flags drugs like benzodiazepines, anticholinergics, and certain NSAIDs. Why? Because they’re more likely to cause falls, confusion, or kidney damage.
Take amitriptyline, an old-school antidepressant. It’s a strong anticholinergic. In younger people, it’s fine. In a 78-year-old with slower liver clearance and reduced kidney function? It can cause extreme drowsiness, dry mouth, urinary retention, and even hallucinations. One Reddit user shared how their 82-year-old mother started on a standard dose and became so dizzy she fell three times in a week. Her doctor didn’t realize the dose needed to be cut in half.
Over-the-counter drugs aren’t safe either. Acetaminophen (Tylenol) is the leading cause of acute liver failure in older adults. Why? Because many seniors take it daily for arthritis, and their liver can’t handle the constant load. The Acetaminophen Hepatotoxicity Registry shows that 50% of cases in people over 65 happen because they didn’t know they were taking too much-sometimes from multiple products that all contain acetaminophen.
Drugs with narrow therapeutic indexes are the most dangerous. That means the difference between a helpful dose and a toxic one is tiny. Warfarin, digoxin, and lithium fall into this category. A small change in liver or kidney function can push levels into the danger zone. That’s why therapeutic drug monitoring-checking blood levels regularly-is critical for these drugs.
What Doctors Should Do (and Often Don’t)
Doctors aren’t ignoring this-they’re overwhelmed. Most were trained in the 1990s, when drug trials rarely included people over 75. Today, 41% of seniors take five or more prescription drugs. That’s polypharmacy. And with each added drug, the risk of interaction and side effects climbs by nearly 90%.
Guidelines exist. The Beers Criteria® recommends starting with 20-40% lower doses for liver-metabolized drugs in patients over 65. For those over 75, reduce even more. The STOPP/START criteria help doctors avoid bad prescriptions and add necessary ones. Studies show using these tools reduces adverse events by 22%.
But here’s the gap: many doctors still use chronological age as the main factor. “She’s 80, so give her half the dose.” That’s not enough. You need to know her liver enzymes, her GFR, her muscle mass, her other medications, and whether she’s taking supplements. That’s complex. And time-consuming.
Tools like GeroDose v2.1, approved by the FDA in 2023, help. It simulates how a drug will behave in a specific patient based on age, weight, liver enzymes, and kidney function. It’s not perfect, but it’s a big step toward precision medicine for seniors.
What You Can Do as a Patient or Caregiver
You don’t need to be a doctor to protect yourself or a loved one. Here’s what works:
- Ask: “Is this medication still necessary?” Many seniors take pills they were prescribed years ago-no one ever reviewed them.
- Ask: “Is this dose right for my age and kidney/liver function?” Don’t assume the same dose is safe.
- Keep a full list of everything you take-prescriptions, OTC meds, vitamins, herbal supplements. Bring it to every appointment.
- Ask for a medication review with a pharmacist. Many pharmacies now offer free medication therapy management for seniors.
- Watch for new symptoms: dizziness, confusion, fatigue, nausea. These aren’t just “getting older.” They could be drug reactions.
- Use one pharmacy. That way, the pharmacist can check for interactions across all your meds.
One 78-year-old man with heart failure and kidney disease was on vancomycin. His dose was based on old formulas. He started feeling sick. His doctor switched to using the CKD-EPI equation for GFR and adjusted his dose. He stayed out of the hospital for a year. Simple change. Big result.
The Bigger Picture
The U.S. spends $30 billion a year treating avoidable drug reactions in older adults. The FDA now requires drug companies to include more older people in trials and analyze results by age. But progress is slow. Only 38% of participants in new drug trials are over 65. That means we’re still guessing how many new drugs affect seniors.
The future? Personalized dosing. Not based on age, but on real-time data: liver enzymes, kidney function, genetic markers, even epigenetic changes. A 2023 study found 17 DNA methylation sites linked to CYP3A4 activity that shift with age. That could lead to blood tests that tell you exactly how your body handles drugs.
By 2030, experts predict these approaches could cut adverse drug events in seniors by 35-50%. But it won’t happen unless patients and caregivers speak up. If your parent is on five meds and feels off, ask questions. Push for a review. Demand better. Because aging doesn’t mean you have to suffer from bad medicine.
Why do older adults need lower doses of some medications?
Older adults often need lower doses because their liver and kidneys don’t process drugs as efficiently. Liver mass and blood flow decrease, slowing drug metabolism. Kidney function drops, reducing drug clearance. This means drugs stay in the body longer, increasing the risk of side effects-even at standard doses.
Can a normal creatinine level mean poor kidney function in seniors?
Yes. Creatinine comes from muscle. As people age, they lose muscle mass, so creatinine levels can stay normal even when kidney function has dropped by 40-50%. That’s why doctors must use formulas like CKD-EPI or Cockcroft-Gault to estimate GFR, not just rely on creatinine alone.
Which common drugs are most dangerous for older adults?
Drugs flagged by the Beers Criteria® include benzodiazepines (like diazepam), anticholinergics (like amitriptyline), NSAIDs (like ibuprofen), and certain sleep aids. These can cause falls, confusion, kidney damage, or liver injury. Even OTC acetaminophen is risky if taken daily without monitoring.
How does polypharmacy increase the risk of side effects?
Taking five or more medications increases the chance of harmful interactions by 88%. Each drug competes for liver enzymes or kidney clearance. Slowed metabolism means drugs build up. Some drugs amplify side effects of others-like combining an antidepressant with a painkiller that both cause drowsiness.
What’s the best way to avoid bad drug reactions in older adults?
Get a full medication review with a pharmacist or geriatrician. Ask if each drug is still needed. Request kidney and liver function tests. Use one pharmacy to catch interactions. Start low, go slow with new prescriptions. Never assume a dose is safe just because it worked years ago.

I had no idea acetaminophen was this risky for seniors 😱 My grandma takes it daily for her knees and I just assumed it was safe. Time to have a talk with her pharmacist ASAP.
So let me get this straight - we’re telling old people to take less medicine because their bodies are falling apart, but the drug companies still test everything on 25-year-old gym bros? Classic. 🤡
This is the kind of stuff that keeps me up at night. My dad’s on five meds and he’s 79. I used to think he was just ‘getting old’ when he’d zone out or stumble. Turns out it was the amitriptyline. We cut the dose in half and he’s like a new man. No more falls. No more confusion. Just him - quiet, calm, and finally comfortable. It’s not about age. It’s about listening. And sometimes, less really is more.
In India, many elderly take whatever the doctor gives without question. But I’ve seen how a simple dose change saved my aunt from kidney trouble. She was on metformin for years - no tests, no reviews. Then her legs swelled up. We got her GFR checked and switched her. She’s walking again. Just because it’s been years doesn’t mean it’s still right.
So the liver shrinks and the kidneys lie about their function and we still give the same pills? Wild
The pharmacokinetic alterations in geriatric populations are profoundly non-linear due to age-related reductions in hepatic blood flow, glomerular filtration rate, and cytochrome P450 enzyme activity. Furthermore, polypharmacy induces competitive inhibition at metabolic sites, resulting in elevated plasma concentrations of substrates with narrow therapeutic indices. The clinical implications necessitate individualized pharmacotherapy protocols predicated on renal and hepatic biomarkers, not chronological age.
I grew up in a household where grandpa took 12 pills a day and no one questioned it. Then one day he started hallucinating. Turns out it was the OTC sleep aid + his blood pressure med. We cut three, swapped two, and now he’s laughing again. I wish we’d known this stuff sooner. Why isn’t this taught in high school? Or at least at the pharmacy counter?
My mother was hospitalized for a drug reaction. They said it was 'just old age.' I called them out. They didn’t have a response. So now I bring a binder to every appointment. With tabs. And color-coded stickers.
The epigenetic modulation of CYP3A4 expression via age-dependent DNA methylation patterns suggests a paradigm shift toward predictive pharmacogenomics in geriatric care. We’re not just dosing by weight or creatinine anymore - we’re entering an era of molecularly calibrated therapeutics. The future is here. Are we ready? 🤖💊
It is imperative that clinicians adopt a more rigorous and evidence-based approach to the prescription of pharmaceutical agents in geriatric populations. The current standard of care, predicated largely on chronological age and anecdotal experience, is insufficient and potentially hazardous. The implementation of validated dosing algorithms and routine therapeutic drug monitoring is not merely advisable - it is ethically obligatory.