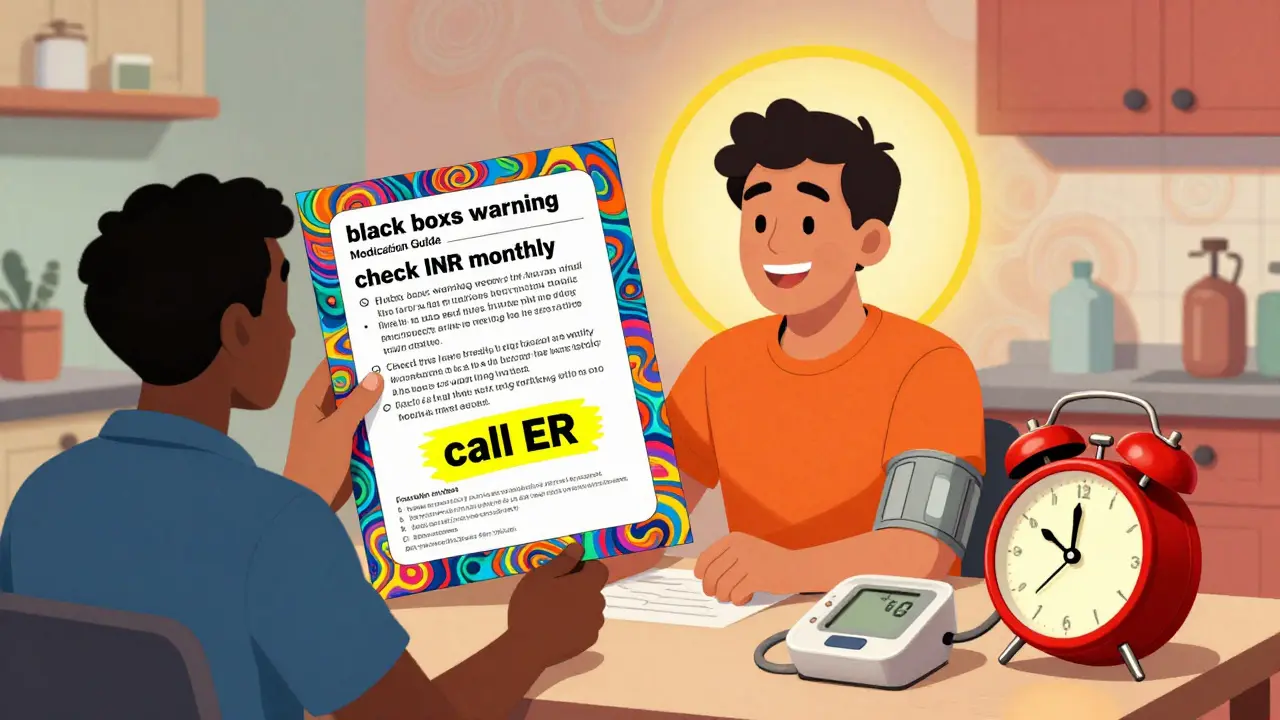
When you pick up a new prescription, you might get a small paper insert tucked into the bottle. It looks simple, but this is a Medication Guide-a legally required document designed to help you avoid serious harm. These aren’t just extra paperwork. They’re your lifeline to understanding what could go wrong, when to watch for it, and what to do next. The FDA requires these guides for drugs with serious, preventable risks. That means if your medication has one, it’s not just about side effects-it’s about life-threatening dangers you can spot early if you know where to look.
What’s in a Medication Guide? It’s Not What You Think
Most people skim these guides like a manual for a toaster. But they’re not written for engineers. They’re written for you-with plain language, bold headers, and real numbers. The FDA mandates that these guides use a 6th- to 8th-grade reading level. No jargon. No fluff. Just clear, urgent information. There are about 150 different guides right now, covering everything from blood thinners to antidepressants to psoriasis treatments. Each one follows the same seven-section structure. The most important parts? The first three.
The first section is titled: “What is the most important information I should know about [drug name]?” This is where the FDA’s black box warnings live. These aren’t vague phrases like “may cause side effects.” They say exactly what’s dangerous: “Can cause serious liver damage,” “May lead to life-threatening blood disorders,” or “Increases risk of heart attack in people over 65.” If your drug has one of these, it’s not optional to read this. It’s critical.
The second section asks: “What should I tell my healthcare provider before taking [drug name]?” This is your checklist. It lists conditions that make the drug unsafe. For example, if you have liver disease, kidney failure, or a history of blood clots, this section tells you whether you should even take the medicine. It also warns about interactions-like “Do not take if you are using alcohol,” or “Avoid this drug if you’re on certain antibiotics.”
Where the Real Monitoring Advice Hides
The third section is the most powerful-and the most ignored. It’s called: “What are the possible or reasonably likely serious side effects of [drug name]?” This is where the monitoring instructions live. This isn’t a list of “maybe” symptoms. It’s a set of concrete actions you must take.
Take warfarin (Coumadin). The guide doesn’t just say “monitor your blood.” It says: “Your healthcare provider should check your INR level at least once a month. If your dose changes, check it more often.” It lists exact symptoms: “Unusual bruising that lasts more than a few days,” “Bleeding from the gums that won’t stop,” “Pink or red urine.” These aren’t guesses. These are signs of internal bleeding you can’t afford to miss.
Antidepressants? They all say the same thing now: “Pay close attention to any changes, especially sudden changes, in mood, behavior, thoughts, or feelings.” And they add: “This is very important when the medicine is started or when the dose is changed.” That’s not general advice. It’s a timer. The first 4-6 weeks are the highest risk window. You need to be watching daily.
Clozapine? The guide says: “About 1 in 200 people taking clozapine may develop agranulocytosis-a condition where your white blood cells drop dangerously low.” Then it tells you: “You must have a blood test every week for the first 6 months.” That’s not a suggestion. It’s a requirement. Skip a test, and you could die without knowing why.
How to Read It Like a Pro
You don’t need a medical degree. You just need a system. Here’s how real patients and pharmacists do it:
- Find the “Most Important Information” section first. Read it out loud. If it scares you, that’s okay. That means it’s working.
- Highlight every word that says “test,” “monitor,” “check,” or “measure.” Use a yellow highlighter. These are your lifelines.
- Circle every time frame. “Weekly,” “monthly,” “before starting,” “every 3 months.” These tell you when to act.
- Underline symptoms that require immediate action. “Call your doctor right away,” “Go to the ER,” “Do not wait.” These are red flags.
Some patients use a “traffic light” system: green for normal, yellow for watchful, red for emergency. If your guide says “unusual bruising,” and you notice it, that’s yellow. If it’s spreading, or you’re bleeding from your nose, that’s red. Call your doctor.
Why Most People Miss the Warning Signs
Studies show 63% of patients misunderstand monitoring instructions. Why? Because they assume “monitor monthly” means “if you feel bad, get a test.” It doesn’t. It means “get tested every month, even if you feel fine.” That’s how serious risks are caught early.
One patient on Reddit said she took a drug for rheumatoid arthritis and skipped her blood tests because she “felt fine.” Three months later, she was hospitalized with liver failure. Her guide said: “Check liver enzymes every 4 weeks.” She didn’t know that “every 4 weeks” meant “on the same day each month,” not “whenever you remember.”
Another common mistake? Assuming the guide is outdated. But the FDA requires manufacturers to update guides within 30 days of new safety data. In 2022, 92% of guides were updated. That means if you’ve had the same drug for years, your guide might have changed. Always check the date on the guide. If it’s older than a year, ask your pharmacist for the latest version.
What to Do If You Don’t Get a Guide
The law says you must get one every time you fill the prescription. But audits show 41% of independent pharmacies fail to hand them out. If you don’t get one, ask for it. Say: “I need the Medication Guide for this drug. It’s required by law.”
If they say they don’t have it, ask them to call the manufacturer. Or go to DailyMed.gov-the NIH’s official database. Type in your drug name. Download the current guide. Print it. Bring it to your next appointment. You have a right to this information.

How to Make It Stick
Reading once isn’t enough. The FDA recommends the 3-2-1 method:
- 3 minutes before your first dose-read the whole guide.
- 2 minutes before each refill-review the monitoring sections.
- 1 minute during treatment-check for changes. Did your doctor change your dose? Did the guide update? If so, re-read the critical sections.
Keep it in your medication journal. Write down your test dates. Set phone reminders. Some patients use a calendar on their fridge. Others use a notes app. The University of Michigan found that patients who recorded their monitoring schedule had 68% fewer adverse events.
What’s Changing in 2026
The FDA is pushing for better design. By 2026, all high-risk medication packages will include QR codes that link directly to the current guide. Some guides are already testing pictograms-simple icons showing when to test or when to call for help. AI tools are being piloted to personalize guides based on your age, other medications, and health history. One system from Pfizer showed a 63% improvement in understanding.
But the biggest change? Medicare is now tying reimbursement to compliance. Pharmacies that don’t hand out guides could lose part of their payment starting in 2025. That means you’re more likely to get one. But you still need to read it.
Medication Guides aren’t perfect. They’re still text-heavy. Some are confusing. But they’re the best tool you have to stay safe. The FDA’s own data shows patients who follow the monitoring advice have 32% fewer serious side effects. That’s not a small number. That’s life or death.
So next time you get a new prescription, don’t toss the guide. Sit down. Read it. Highlight it. Mark the dates. Ask questions. You’re not just reading a pamphlet. You’re reading your safety plan.
Are Medication Guides the same as the package insert?
No. The package insert is a technical document meant for doctors and pharmacists. It’s full of medical jargon and detailed data. Medication Guides are the plain-language version created specifically for patients. They focus only on serious risks and monitoring steps. You’ll get both, but only the guide is required by law to be handed to you.
What if I don’t understand a warning in the guide?
Don’t guess. Ask your pharmacist or doctor. Bring the guide with you. Say: “I don’t understand what ‘get blood tests regularly’ means-how often is that?” Pharmacists are trained to explain these guides. They’ve seen hundreds of patients struggle with the same lines. There’s no shame in asking. In fact, it’s the smartest thing you can do.
Do all prescription drugs have Medication Guides?
No. Only drugs with serious, preventable risks get them. That includes blood thinners, antidepressants, immunosuppressants, and certain cancer drugs. About 150 medications currently require one. If your drug doesn’t have a guide, it means the FDA doesn’t consider the risks severe enough to require this level of patient warning. That doesn’t mean it’s risk-free-just that the danger isn’t as immediate or preventable with patient monitoring.
Can I get a Medication Guide online?
Yes. Go to DailyMed.gov, run by the National Institutes of Health. Search for your drug name. You’ll find the current, official Medication Guide in PDF format. You can download, print, or save it to your phone. This is especially helpful if your pharmacy didn’t give you one, or if you lost it. The guide on DailyMed is updated in real time when the FDA requires changes.
What if my medication’s guide changes while I’m taking it?
The FDA requires manufacturers to update guides within 30 days of new safety data. If your guide was updated, your pharmacy should give you the new version with your next refill. But don’t wait. Check DailyMed.gov every 6 months. If you see a new warning-especially one about monitoring or symptoms-you need to know. A change in the guide could mean a new risk you didn’t know about. Don’t assume your old info is still valid.

Comments
Post Comment