
Snoring isn’t just annoying-it’s a sign your airway is collapsing while you sleep. For millions of people, it’s not just about keeping the peace with a partner. It’s about breathing. And when CPAP machines feel like a prison, many are turning to something smaller, quieter, and easier to live with: oral appliance therapy.
What Is Mandibular Advancement for Snoring?
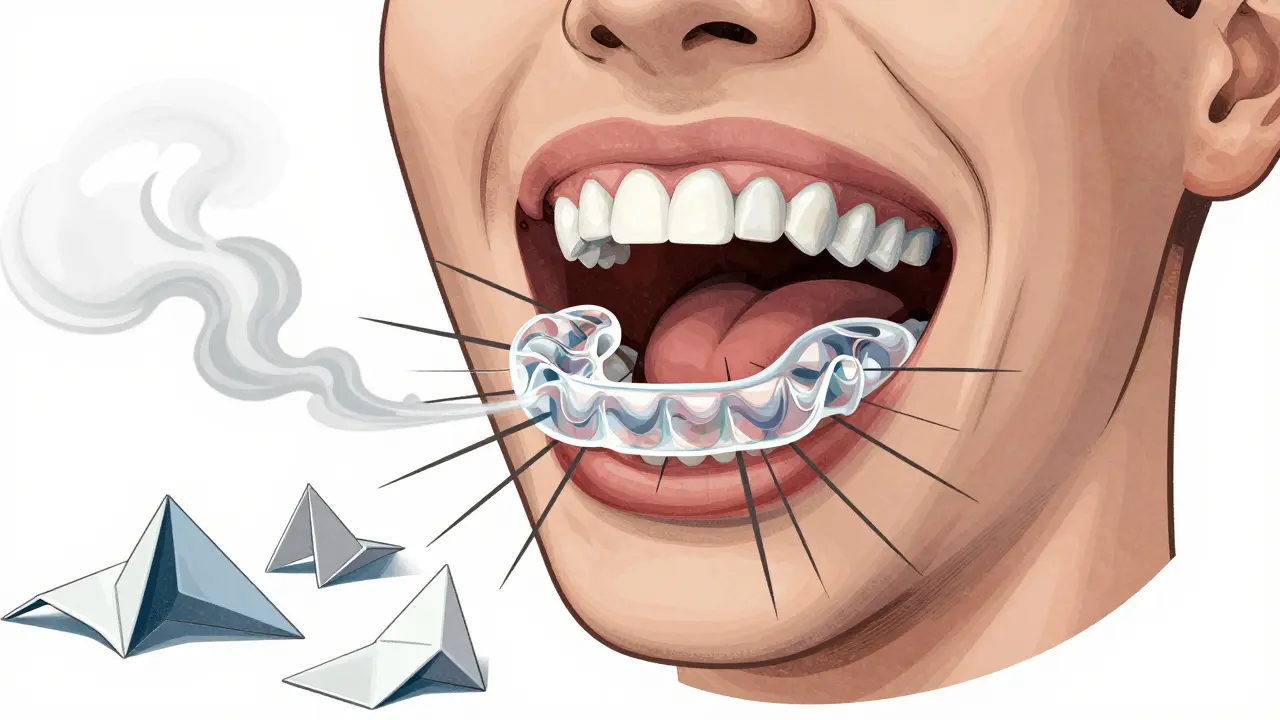
Oral appliance therapy (OAT) uses a custom-fitted device worn in the mouth during sleep to gently push the lower jaw forward. This movement pulls the tongue and soft tissues away from the back of the throat, keeping the airway open. The device is called a Mandibular Advancement Device, or MAD. It doesn’t cure snoring, but it stops it for most people who use it correctly. Unlike CPAP, which blasts air through a mask, MADs work mechanically. There’s no hose, no noise, no claustrophobia. Just a small plastic appliance, about the size of a mouthguard, that fits snugly over your teeth. It’s why nearly 1.8 million Americans now use them, up from just 5% of snorers in 2015 to over 14% today.How Do These Devices Actually Work?
The science is simple: when your jaw moves forward, your tongue follows. That’s it. The space behind your tongue-where most snoring happens-is no longer blocked. Studies show that advancing the jaw by 8 to 10 millimeters reduces snoring intensity by 60% to 75% in most users. Custom devices are made from semi-rigid acrylic with titanium connectors. They’re built from dental impressions taken in a dentist’s office. Over-the-counter versions, like Zyppah or Good Morning Snore Solution, use thermoplastic material you boil and bite into. But here’s the catch: custom devices work twice as well. A 2015 meta-analysis found custom MADs reduced snoring by 72.3%, while OTC models only hit 48.6%. The best devices let you adjust the jaw position in small steps-0.5mm at a time. Most people need to tweak it over a few weeks until snoring stops. Too little, and it won’t help. Too much, and your jaw aches. Finding the sweet spot takes patience.Who Benefits Most From This Treatment?
Not everyone is a candidate. The American Academy of Sleep Medicine recommends MADs for people with primary snoring or mild-to-moderate obstructive sleep apnea (OSA). If you have severe OSA, CPAP is still the gold standard. MADs fail in about 39% of those cases, especially if your airway is completely collapsed (Mallampati Class IV). You also need enough healthy teeth. Most devices require at least 6-8 natural teeth in each arch to grip onto. If you wear full dentures, have severe gum disease, or have a history of TMJ pain, you’re probably not a good fit. About 13% of snorers are ruled out after a dental exam. The best candidates are people who:- Snore loudly but don’t stop breathing often
- Can’t tolerate CPAP due to discomfort or claustrophobia
- Travel often and need something portable
- Have mild weight gain or sleep on their back
How Does It Compare to Other Treatments?
Let’s be clear: MADs aren’t perfect. But they’re better than most alternatives. - CPAP stops snoring in 85-95% of cases, but only about half of users stick with it after a year. The mask leaks, the hose tangles, and the noise drives partners crazy. MADs win on compliance-76% of users wear them nightly after 12 months. - Nasal strips and nasal dilators help maybe 20-30% of people. They only open the nose, not the throat. Snoring often continues. - Positional therapy (sleeping on your side) works for 35-45% of people. But it’s hard to maintain. You roll over in your sleep. - Surgery like UPPP removes tissue from the throat. It’s invasive, painful, and doesn’t always work. MADs are reversible. Take it out, and your jaw goes back to normal. MADs sit in the middle: not as powerful as CPAP, but way easier to use. That’s why sleep specialists call them the only non-surgical, evidence-backed solution for primary snoring.What Are the Side Effects?
No treatment is without trade-offs. About 25% of long-term MAD users develop dental changes. Your bite might shift. Teeth can feel loose. Some need braces or crowns years later. Short-term issues are more common:- Morning jaw pain (68% of users in the first week)
- Excessive saliva (43%)
- Tooth discomfort (29%)
- Dry mouth or sore gums
How Much Does It Cost?
Custom MADs cost between $1,800 and $2,500. That includes the dentist visit, impressions, device, and follow-ups. Insurance rarely covers it-only 38% of U.S. plans pay anything. Many people pay out of pocket. Over-the-counter versions cost $99-$150. They’re tempting. But they’re less effective, less durable, and often don’t fit right. A 2022 study found at-home impression kits led to 23% worse fit than in-office digital scans. Follow-up visits with a dental sleep specialist run $150-$300 each. You’ll need 2-3 over the first 3-6 months. Some practices include them in the upfront price.
How Do You Get Started?
Step 1: Rule out sleep apnea. See a sleep specialist. Get a home sleep test. If you have severe OSA, MADs won’t cut it. Step 2: Visit a dentist trained in dental sleep medicine. They’ll check your teeth, jaw, and airway. If you’re a candidate, they’ll take impressions or a digital scan. Step 3: Get fitted. Your device will be ready in 2-3 weeks. Step 4: Titrate. Adjust the jaw position slowly-1mm every 3-5 days-until snoring stops. Most people reach their ideal setting in 4-6 weeks. Step 5: Maintain. Clean the device daily with mild soap and water. Brush your teeth before putting it in. See your dentist every 6 months to check for tooth wear or bite changes.What’s New in 2026?
The field is evolving fast. In 2023, the FDA cleared the SomnoDent EVO 3, a MAD with built-in sensors that connect to an app. It tracks how often you wear it and how much your jaw moves. Next year, Sleep Solutions Inc. is launching a device with AI that adjusts the jaw position automatically based on your snoring patterns. Researchers are also exploring genetic markers to predict who will respond best to MADs. In five years, your treatment might be tailored to your DNA, not just your jaw size.Is It Worth It?
If you snore and hate CPAP, yes. If you’ve tried everything else and your partner is losing sleep, yes. If you’re willing to invest time, money, and a little discomfort for a better night’s rest, yes. It’s not magic. It’s medicine. And like any medicine, it works best when you use it right.Can oral appliances cure snoring permanently?
No. Snoring returns within 48 hours of stopping use. MADs manage the condition, not cure it. They’re like glasses for your airway-you need to wear them to keep breathing properly.
Are over-the-counter snoring devices worth buying?
They’re better than nothing, but not as good as custom devices. OTC models reduce snoring by about half as much and often cause jaw pain because they don’t fit well. If you’re serious about stopping snoring, invest in a custom MAD.
Do I need a sleep study before getting a MAD?
Yes. Many people who snore also have sleep apnea. A home sleep test rules out moderate or severe OSA. Treating snoring alone without checking for apnea can be dangerous.
How long do oral appliances last?
Custom MADs last 3-5 years with proper care. OTC devices often break or lose shape in under a year. Wear and tear from grinding or clenching can shorten lifespan.
Will my insurance cover an oral appliance for snoring?
Only if you have diagnosed obstructive sleep apnea. Most insurers won’t cover MADs for primary snoring alone. Always check with your provider before spending money.
Can children use mandibular advancement devices?
No. These devices are designed for adults with fully developed jaws. Children with snoring issues should be evaluated for tonsil or adenoid problems, not fitted with MADs.
What if I have braces or dental implants?
Braces usually aren’t a problem, but your dentist needs to adjust the device around them. Implants are often fine-they can even serve as anchors. But if you have multiple missing teeth, you may not be a candidate.


i got one of those otc mouthpieces off amazon last year. thought it was gonna be magic. woke up with a jaw like i’d been clenching a baseball bat all night. still snore. just quieter now. and my dentist said i’m grinding my molars into dust. worth the $120? maybe. worth my sleep? not even close.
in india, most people don’t even know this exists. we have a guy in our village who snored so loud the neighbors called the police. he tried nasal strips, saltwater rinses, even sleeping on a pile of coconuts (true story). last month he finally saw a dentist who mentioned this thing. he’s getting a custom MAD next week. if it works, i’m gonna start a campaign to get these into rural clinics. imagine if every snorer in a 50km radius could sleep without waking the whole block. we need more awareness, not just more masks.
why are we treating snoring like it’s a disease? it’s just biology. people snore. get over it. if your partner snores, get earplugs. or sleep in another room. stop spending $2k on plastic mouthguards like it’s some kind of biohacking trend. this is just capitalism selling you a solution to a problem you could’ve solved with a pillow.
oh wow. another ‘sleep solution’ that costs more than my monthly rent. 🤦♀️ next they’ll sell us a $3000 tongue tether. if you’re spending $2k to stop snoring, you’re either rich or desperate. and if you’re desperate, you’re probably also apneic and haven’t gotten the test yet. just say no. buy a fan. sleep on your side. cry into your pillow. it’s cheaper and less likely to ruin your teeth.
i’ve been using a custom MAD for 18 months now. it changed my life. before, my wife would wake up 4-5 times a night. now she sleeps through. yes, my jaw ached at first. yes, i had to adjust it slowly. yes, i had to pay out of pocket. but i didn’t need surgery. i didn’t need a machine that sounds like a jet engine. i just needed something that fits. if you’re considering this, talk to a sleep dentist. don’t just buy something off the internet. the difference is night and day.
my mum had one of these after her sleep study. she was skeptical too-thought it’d be gross. but after two weeks, she said it felt like her mouth was finally ‘in the right place.’ no more waking up with a dry throat. she even started sleeping on her back again. weirdly, it helped her acid reflux too. the dentist said jaw position affects the esophagus. who knew? i’m glad she didn’t give up.
so let me get this straight. you’re telling me i can pay $2k to wear a mouthguard so my wife doesn’t throw a pillow at my head… but if i just sleep on my side, it’s ‘lazy’? i’ve tried every gimmick. nasal strips? useless. chin straps? made me look like a robot. this thing? it’s the only thing that didn’t make me feel like i was wearing a sci-fi prop. i’m not a medical genius. i’m just a guy who wants to sleep without being called a dragon at 3am.
if you’re not american, you don’t understand this. in the us, everything is a product. snoring? product. sleep? product. your ability to breathe? product. we’re not even talking about health anymore. we’re talking about branding. this isn’t medicine. it’s a luxury accessory for people who can afford to treat their biology like a subscription service.
you people are so gullible. this isn’t science. it’s dentists making money off your ignorance. if you had real sleep apnea, you’d be on cpap. if you don’t, you don’t need a device. you need to lose weight. or stop drinking. or sleep on your side. but nooo, let’s just shove plastic in our mouths and call it innovation. this is why america is broke.
the real problem is that no one admits that 80% of snoring is caused by being overweight. but hey, let’s sell a $2000 gadget instead of telling people to eat less bread. this whole thing is a scam wrapped in clinical jargon. if you’re snoring, check your bmi before you check your dentist’s calendar.
Just wanted to add-when you get your custom device, make sure the dentist does a full occlusion check. I didn’t, and after six months, my bite shifted so bad I needed a night guard AND a retainer. It’s not just about snoring. It’s about your entire dental structure. Don’t skip the follow-ups. They’re not upsells. They’re necessary. And yes, clean it daily. I use a soft toothbrush and dish soap. No toothpaste-it’s too abrasive. Trust me.
my husband got one of those otc ones because he didn’t want to ‘waste money’ on a dentist. lasted three weeks. then he lost it on a road trip. he’s still mad he didn’t get the custom one. i’m just glad he stopped snoring for a little while. now he’s finally considering the real thing. i told him if he buys it, i’ll buy him a new pillow. he said that’s not fair. i said: ‘you’re the one who sounds like a chainsaw in a blender.’
does anyone know if these work for people with sleep apnea who also have TMJ? my jaw clicks when i open my mouth, and my doctor says i’m a candidate for MADs. but my dentist says ‘maybe not.’ i’m stuck in medical limbo. any real experience here? i just want to sleep without my wife leaving the house.
ohhh so now we’re giving out gold stars to people who spend $2k on a mouthguard? congrats, you didn’t die from snoring. big win. meanwhile, people in other countries are using a rolled-up sock and a prayer. this is why america is the most expensive place to be mildly inconvenienced. if your snoring is so bad you need a $2k device, maybe you should’ve stopped eating fried chicken at 2am. just saying.