Beta-Blocker Safety Checker for Asthma Patients
Is Your Beta-Blocker Safe for Asthma?
Enter the name of your beta-blocker medication to check if it's safe for asthma patients. This tool is based on current medical guidelines.
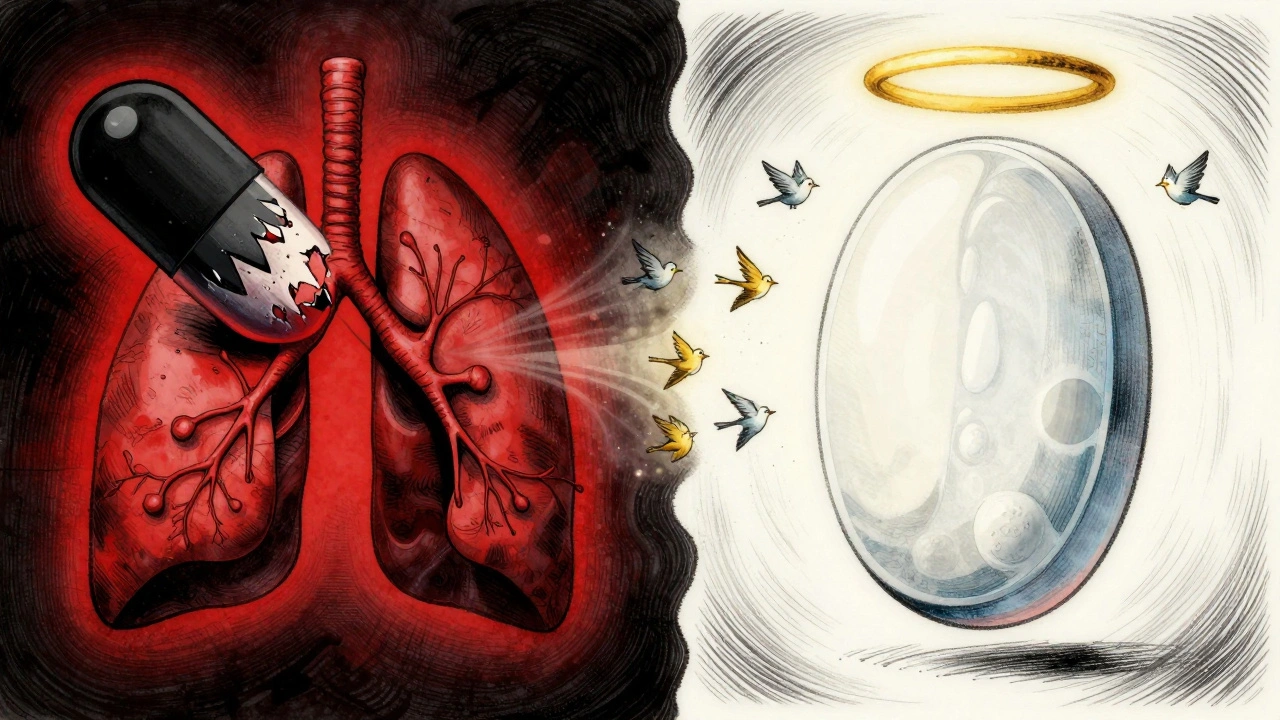
For years, doctors told asthma patients to avoid beta-blockers at all costs. The warning was simple: these heart medications could trigger a life-threatening asthma attack by tightening your airways. But today, that advice is changing - and the difference isn’t just subtle, it’s life-saving for many.
Why Beta-Blockers Were Banned for Asthma Patients
Beta-blockers work by blocking adrenaline, which slows your heart rate and lowers blood pressure. That’s why they’re used after heart attacks, for high blood pressure, and to manage irregular heartbeats. But early versions like propranolol didn’t just target the heart. They hit every beta receptor in the body - including those in your lungs.Those lung receptors, called beta-2 receptors, help keep your airways open. When blocked, they cause bronchoconstriction - the same thing that happens during an asthma flare-up. That’s why a single dose of propranolol could drop lung function by 10%, according to clinical studies. And if you were already wheezing or struggling to breathe, it could push you into a full-blown attack.
That’s why guidelines like the British National Formulary (BNF) said: avoid beta-blockers in asthma. It wasn’t just a suggestion - it was a hard rule. And for decades, it kept people safe.
The New Science: Not All Beta-Blockers Are the Same
Here’s the twist: not all beta-blockers are created equal. Over the past 30 years, researchers discovered that some beta-blockers are cardioselective. That means they mostly stick to beta-1 receptors in the heart and leave the beta-2 receptors in your lungs alone.These include atenolol, metoprolol, bisoprolol, and others. Studies show they’re far less likely to cause trouble. In one review of 29 trials involving asthma patients, cardioselective beta-blockers caused only a 7.5% drop in lung function - and that drop vanished completely after using an albuterol inhaler. No one had worsening symptoms. No hospitalizations. No deaths.
Compare that to non-selective beta-blockers like propranolol or nadolol, which caused a 10% drop in lung function - and sometimes triggered real breathing problems. That’s why labetalol and timolol are still off-limits for asthma patients.
Atenolol: The Safest Choice for Asthma Patients
When researchers directly compared atenolol and metoprolol in 14 asthma patients with high blood pressure, atenolol came out ahead. Patients on atenolol had fewer asthma attacks, more asthma-free days, less wheezing, and better evening lung function. The difference was statistically significant - meaning it wasn’t by chance.Why? Atenolol is more selective for the heart than metoprolol. It barely touches the lungs, even at higher doses. A 2022 review in the European Journal of Clinical Pharmacology specifically recommended atenolol as the preferred beta-blocker for asthma patients who need heart protection.
And here’s something surprising: no deaths or severe bronchospasms have ever been reported in the medical literature from cardioselective beta-blockers in asthma patients - even after hundreds of exposures.
How Doctors Are Changing Their Approach
The American Academy of Family Physicians now says cardioselective beta-blockers are safe for people with mild to moderate asthma. The Primary Care Notebook confirms they don’t worsen COPD or asthma symptoms over time. Even the BNF, once the strictest voice, now says: if you absolutely need a beta-blocker - and your asthma is well-controlled - you can use one, but only under specialist supervision.So what does that look like in real life?
- Start with the lowest possible dose - often half the usual starting dose.
- Use atenolol if possible. If not, metoprolol or bisoprolol are acceptable alternatives.
- Never use propranolol, nadolol, or timolol.
- Monitor lung function with a spirometer before starting and again after two weeks.
- Make sure your rescue inhaler (albuterol) is always within reach.
One study gave bisoprolol daily for two weeks to 19 asthma patients. Their lung function stayed stable. When they needed albuterol for a flare-up, it worked just as well as before. That’s huge - it means your emergency treatment still works, even if you’re on a beta-blocker.
What About Long-Term Use? Is It Safe?
Here’s another twist: long-term use might actually help your lungs. Animal studies show that while beta-blockers can make airways more sensitive at first, over weeks or months, they reduce inflammation and lower airway hyperresponsiveness. In other words, your lungs might get calmer over time.One study even found that celiprolol - a special cardioselective beta-blocker - didn’t just avoid causing bronchoconstriction. It actually blocked the airway-tightening effects of propranolol. That’s like having a bodyguard for your lungs.
That’s why doctors now think of beta-blockers not just as heart drugs, but as potential long-term protectors - even for the lungs.
What You Should Do If You Have Asthma and Need a Beta-Blocker
If you’re on a beta-blocker and have asthma, here’s what matters:- Know which one you’re taking. If it’s propranolol, nadolol, or timolol - talk to your doctor immediately. These are not safe for asthma.
- Ask about switching. If you’re on a non-selective beta-blocker and have asthma, ask if you can switch to atenolol. It’s not a gamble - it’s backed by solid data.
- Don’t stop your beta-blocker cold. Stopping suddenly can trigger a heart attack or dangerous spike in blood pressure. Always work with your doctor to switch safely.
- Keep your inhaler handy. Even with a cardioselective beta-blocker, your asthma might flare under stress, illness, or extreme cold. Always have your rescue inhaler with you.
- Get lung tests. A simple spirometry test before and after starting the medication can tell you if it’s affecting your breathing. It takes five minutes.
What If You’re Already on a Beta-Blocker and Your Asthma Gets Worse?
If you’ve been on a beta-blocker and notice more wheezing, more frequent attacks, or your inhaler isn’t working as well - don’t assume it’s just your asthma getting worse. It might be the medication.Call your doctor. Ask for a lung function test. Ask if you’re on a cardioselective beta-blocker. If you’re not, ask if switching is an option. The data is clear: you don’t have to choose between heart health and breathing.
The Bottom Line
The old rule - “beta-blockers are dangerous for asthma” - is outdated. It was based on the wrong drugs. Today, we know better.Cardioselective beta-blockers like atenolol are not just safe - they’re often the best choice for asthma patients who need heart protection. They reduce the risk of death after a heart attack by up to 34%. And they don’t wreck your lungs.
You don’t have to live in fear. You don’t have to give up heart medication to breathe easier. You just need the right drug, the right dose, and the right doctor guiding you.
If you have asthma and a heart condition, ask your doctor: "Is my beta-blocker cardioselective? Could I switch to atenolol?" That one question could change your life.

I read this and just shrugged. My inhaler works fine. My heart meds work fine. Why is this even a thing?
So let me get this straight we spent 50 years telling people not to take beta-blockers because they might kill them and now we're saying oh wait never mind just use the fancy ones and don't worry about it? Classic medicine. First we panic then we shrug. And we wonder why people don't trust doctors
The clinical evidence presented is methodologically sound and aligns with contemporary meta-analytic reviews published in peer-reviewed journals between 2018 and 2023. The cardioselectivity profile of atenolol demonstrates a statistically significant reduction in bronchial reactivity compared to non-selective antagonists. It is imperative that primary care providers recalibrate prescribing paradigms in accordance with updated guidelines from the American Academy of Family Physicians and the British National Formulary.
I've been on metoprolol for 3 years with mild asthma and never had an issue. My pulmonologist said it was fine. Why do people still act like beta-blockers are poison? We're not living in 1985 anymore.
This is the kind of info that actually saves lives 🙌 I used to be scared to even take a cold medicine because I thought it would trigger my asthma now I'm on atenolol and my lungs feel better than ever. Doctors need to stop scaring people and start telling the truth
I think it's really important that we recognize how much the medical community has evolved on this issue and how many people have been needlessly afraid for decades because of outdated guidelines and fear based prescribing practices and even though we now have better data and better drugs the stigma still lingers and it's not just about the medication it's about how we communicate risk and safety and trust and that's the real challenge not the science
I'm a nurse and I've seen patients panic because they were told beta-blockers were forbidden. Then they get switched to atenolol and they cry because they can finally sleep again without wheezing. It's not just about the drug it's about dignity and peace of mind. We owe it to people to update our knowledge
You're all missing the point. What if someone has both asthma and severe heart failure? Atenolol might be safer for lungs but it's weaker for the heart. You're acting like this is black and white. Medicine is gray. And if you think one drug fits all you're not thinking like a doctor you're thinking like a Reddit post
I love how this post breaks it down simply but deeply. I'm from India and here too many doctors still avoid beta-blockers in asthma patients out of habit. I shared this with my cousin who was on propranolol and now she's on atenolol. She says she feels like a new person. This isn't just science it's freedom. Keep spreading this message