
When a brand-name drug loses its patent, prices usually drop by 80% or more. That’s the rule. But what happens when the company that made the brand-name drug also starts selling the generic version? It’s not a trick. It’s called an authorized generic, and it’s one of the most strategic moves in pharmaceuticals today.
What Exactly Is an Authorized Generic?
An authorized generic is the exact same pill, capsule, or injection as the brand-name drug-same active ingredient, same inactive ingredients, same size, same color, same manufacturing process. The only difference? The label. It doesn’t say Pfizer, Eli Lilly, or AstraZeneca. It says something like "Omeprazole 20 mg" and carries the name of a subsidiary or distributor. The FDA requires this. Trademark law stops a company from selling the exact same packaging as the brand. So they change the label, the box, maybe the imprint code on the pill. But inside? Identical. That’s why patients often can’t tell the difference-even if they’ve been taking the brand for years. The first big case happened in 1997 when AstraZeneca launched an authorized generic of Prilosec (omeprazole) the day its patent expired. Within six months, they captured 30% of the entire omeprazole market. That’s not luck. That’s strategy.Why Do Brand Companies Do This?
Think about it: when a patent expires, dozens of companies rush in to make cheaper versions. Prices crash. Revenue plummets. In some cases, a drug that made $1 billion a year drops to $100 million in 12 months. Instead of watching their profits disappear, brand manufacturers play defense. They launch their own generic version. Now they’re not just competing against others-they’re one of the others. And because they already know how to make the drug, they can get it to market faster than anyone else. The FDA says it takes traditional generic manufacturers an average of 17 months to get approval. Brand companies? They can launch an authorized generic in 6 to 9 months. Why? Because they already have all the data. They’ve already passed every inspection. Their facility is already FDA-approved. They don’t need to start from scratch. This also lets them skip the 180-day exclusivity period that’s given to the first traditional generic applicant. That means they can launch on day one-right alongside the competition. In 2019, Teva did this with Copaxone. On the exact day the patent expired, their authorized generic hit shelves. They captured 22% of the market in the first quarter.How Is It Made?
The production line doesn’t change. Same factory. Same machines. Same workers. The same batch of active pharmaceutical ingredient (API) that went into the brand-name drug now gets repackaged under a different label. The only real work is administrative:- File an Abbreviated New Drug Application (ANDA) under a subsidiary name
- Update labeling to remove brand names and logos
- Set up a separate sales team to avoid mixing marketing channels
- Coordinate with distributors and pharmacies to ensure the generic is stocked
What’s the Impact on Prices?
Here’s where it gets complicated. On paper, authorized generics are cheaper than the brand. Usually 10% to 15% lower. But they’re still 5% to 10% more expensive than the traditional generics made by other companies. That creates a strange pricing tier:- Brand: $120/month
- Authorized generic: $105/month
- Traditional generic: $30/month
Is This Fair?
The Federal Trade Commission (FTC) thinks not. Between 2015 and 2020, the FTC sued several companies for using authorized generics as a way to block real competition. In 2017, they won a $448 million settlement against Actavis over Namenda, arguing the company introduced its own generic to scare off other manufacturers. The argument? If you’re the only company that can make the drug, and you’re the one launching the "generic," you’re not creating competition-you’re controlling it. PhRMA, the big drug industry group, disagrees. They say authorized generics increase access and maintain quality. They point to FDA data showing 99.7% bioequivalence between brand and authorized generic drugs. The Congressional Budget Office estimates authorized generics save $2.3 billion a year in drug spending. Sounds good. But they also say that’s only 37% of what could be saved if traditional generics had a fair shot.Who Benefits?
The brand manufacturers? Definitely. They protect their revenue. They keep their factories running. They avoid layoffs. They maintain control over distribution. Pharmacies and insurers? Sometimes. Authorized generics are easier to stock. They don’t have to retrain staff. They know the product. But they don’t get the deepest discounts. Patients? It depends. If you care about price, you lose. If you care about consistency, you win. Many patients report fewer side effects with authorized generics compared to traditional ones-even though they’re supposed to be identical. Why? Maybe it’s placebo. Maybe it’s real. Either way, the perception matters.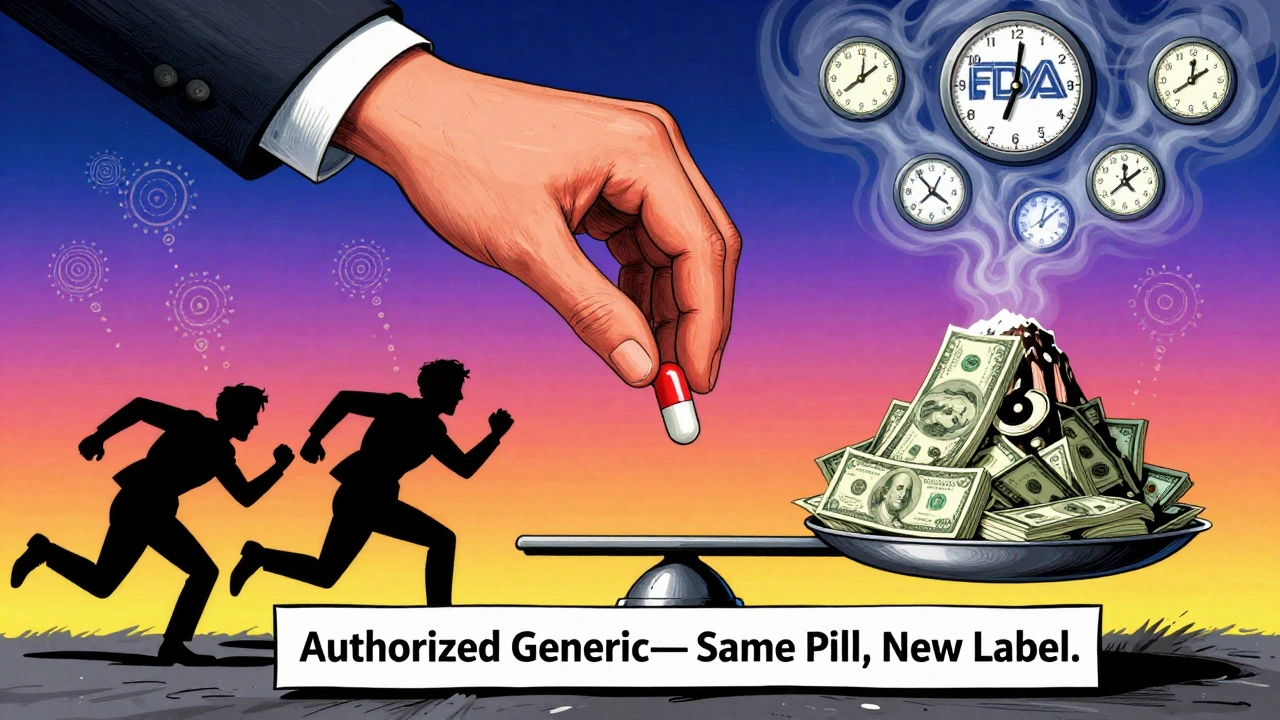
The Bigger Picture
Between 2023 and 2027, $250 billion worth of brand-name drugs will lose patent protection. That’s a tsunami of expirations. The top five pharma companies-Pfizer, Johnson & Johnson, Roche, Merck, AbbVie-launched 47 authorized generics between 2020 and 2023. That’s a 28% increase year over year. And it’s spreading beyond pills. In 2023, Johnson & Johnson launched the first authorized generic of a long-acting injectable drug, Invega Sustenna. That’s huge. Injectables are harder to copy. Manufacturing them requires specialized equipment. Fewer companies can do it. Now, the first authorized biosimilar is here. Amgen launched its own version of Enbrel in 2023. That’s a biologic-a complex protein-based drug. If they can make an authorized biosimilar, what’s next? Analysts predict that by 2025, 40% of small-molecule drugs losing patents will have authorized generics. That’s not a trend. That’s the new normal.What Should You Know as a Patient?
If you’re on a brand-name drug and it goes generic:- Ask your pharmacist: "Is this the authorized version?"
- Check the label. If it has the same name as your brand, it’s probably authorized.
- Compare prices. The real generic is often half the price.
- Don’t assume "generic" means cheaper. Sometimes it means "same company, different label."



It’s wild how the system lets a company essentially create a monopoly under the guise of competition. The authorized generic isn’t competition-it’s camouflage. Patients think they’re saving money, but they’re just paying less than the brand, not the real generic price. The real losers are the people who can’t afford to be confused by labeling.
Of course they do this. The whole pharma industry is a pyramid scheme built on patents and fear. They don’t make drugs to heal-they make them to extract. Authorized generics? Just the latest way to suck more blood from the patient’s wallet while pretending to be the good guy.
Let’s not pretend this is a market failure-it’s a legal one. The Hatch-Waxman Act was never meant to enable this. The FDA’s 99.7% bioequivalence stat is meaningless when the pill’s identical and the price isn’t. They’re gaming the system with bureaucratic loopholes. And the FTC? They’re toothless. This isn’t capitalism-it’s corporate feudalism.
I’ve been following this for years, and honestly, the most fascinating part is how the manufacturing infrastructure doesn’t change at all. Same factory, same workers, same API batch-just a different label and a different subsidiary name on the paperwork. It’s like a magician switching hats while the trick stays exactly the same. The real cost isn’t production-it’s the legal and administrative overhead of pretending you’re not the same company. And yet, companies still do it because the ROI is insane. They recoup $20 million in 14 months by keeping 30% of the market that would’ve otherwise gone to real generics. That’s not innovation, that’s financial engineering disguised as pharmaceutical strategy.
The authorized generic is the ultimate neoliberal paradox: a product that is functionally identical yet economically distinct. It’s not a generic-it’s a *rebranded monopoly*. The pharma titans have weaponized consumer trust. Patients aren’t choosing based on efficacy-they’re choosing based on brand equity, even when the brand is just a ghost. This isn’t healthcare-it’s behavioral economics wrapped in a pill bottle.
Let’s be clear: this isn’t a loophole-it’s a backdoor coup. The Hatch-Waxman Act was designed to encourage competition, not to let the monopolist become the sole competitor. When the same entity controls both the brand and the "generic," you don’t have a market-you have a puppet show. The FTC’s $448M settlement against Actavis was a slap on the wrist. What we need is structural reform: ban authorized generics outright. Let the market work-or don’t pretend it’s working at all.
so like… if i buy the "generic" and its the same pill as my brand but cheaper… why am i paying more for the one with the same name? i feel like my pharmacist is hiding something. also i think my anxiety is just because i dont know if i’m getting the real thing or the fake fake thing
As someone from India where generics are the norm, this whole thing feels so… American. We don’t care who made it as long as it works. But here, people pay extra for the same pill because it has a familiar name? That’s not science-that’s branding. And honestly? It’s kind of sad.
Big Pharma is a foreign cartel and this is just another way they bleed American taxpayers. Why does the government let them do this? Because they own Congress. End of story.
This is actually a great example of how companies can adapt without being predatory. Yes, they’re protecting revenue-but they’re also keeping jobs, maintaining quality, and giving people an option that’s familiar. If you want the cheapest price, go for the traditional generic. If you want peace of mind, the authorized one’s there. It’s not evil-it’s business. And honestly? I’d rather have a company that stays in the game than one that bails and leaves patients stranded.
My grandma takes omeprazole and she swears the brand is better even though she’s been on the generic for years. She says the pills feel different. Maybe it’s placebo. Maybe it’s the packaging. But she’s happier. And if that means she takes it consistently? That’s a win. Sometimes medicine isn’t just chemistry-it’s comfort.
It is imperative to recognize that the authorized generic model, while economically advantageous for manufacturers, does not inherently compromise pharmaceutical integrity. The bioequivalence data, as affirmed by the FDA, is robust and incontrovertible. Furthermore, the continuity of supply chain and manufacturing standards ensures that patient safety remains uncompromised. Therefore, while price differentials exist, the ethical imperative lies in ensuring access-not in artificially depressing prices at the expense of systemic stability.
Just read this whole thing. I’m not even mad anymore. I’m just… exhausted. This is the system. It’s not broken. It’s working exactly as designed. And the worst part? We all play along. We buy the authorized generic because we don’t know better. We don’t ask. We don’t push back. We just take the pill. And the company? They’re smiling all the way to the bank.