
When you pick up a prescription, you might see two names on the label: one you recognize, like Lyrica, and another you’ve never heard of, like pregabalin. The second one is the generic version - and it’s almost always cheaper. But how much cheaper? And does it work just as well? The answer isn’t just about saving a few dollars - it’s about billions in savings for the whole U.S. healthcare system.
Generics Are Just as Effective - But Cost a Fraction
The FDA requires that generic drugs be bioequivalent to their brand-name counterparts. That means they have the same active ingredient, strength, dosage form, and route of administration. They must also deliver the same amount of medicine into your bloodstream at the same rate. In simple terms: if your brand-name pill works, the generic version works the same way.
It’s not a guess. It’s science. The FDA tests generics using strict standards - typically requiring blood levels to stay within 80% to 125% of the brand’s levels. Over 98% of approved generics are rated "AB" in the FDA’s Orange Book, meaning they’re therapeutically equivalent. That’s not a small detail - it’s the foundation of why generics save so much money without sacrificing safety.
And the cost difference? It’s staggering. In 2022, the average copay for a generic prescription was $6.16. For the brand-name version of the same drug? $56.12. That’s more than nine times more. For some medications, like sertraline (generic for Zoloft), patients report paying $9 for the generic versus $450 for the brand. That’s not a typo. That’s the reality for people on high-deductible plans or without insurance.
Generics Are the Backbone of U.S. Prescription Spending
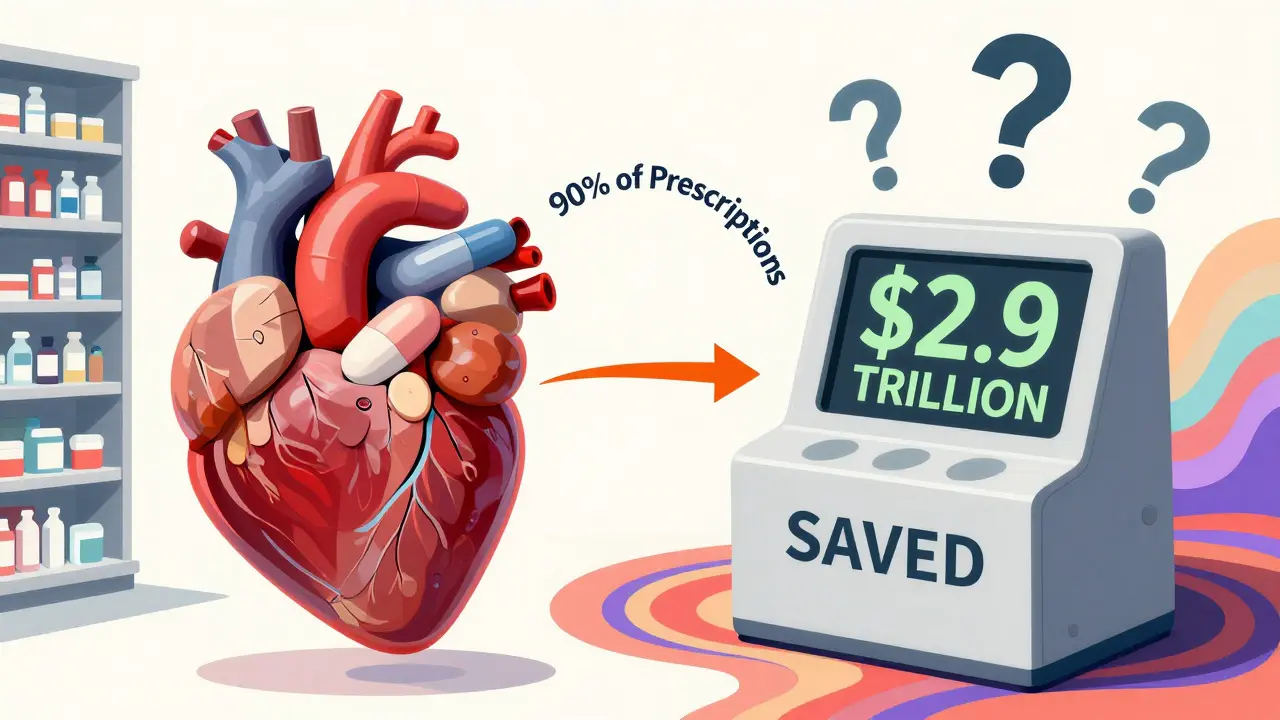
Here’s the most surprising part: generics make up 90% of all prescriptions filled in the U.S. - but they account for only 1.5% of total drug spending. Meanwhile, brand-name drugs make up just 10% of prescriptions but consume nearly 82% of the money spent on prescriptions.
This isn’t new. Since the 1984 Hatch-Waxman Act created a faster approval path for generics, the system has been designed to encourage competition. When a patent expires, other companies can make the same drug without repeating expensive clinical trials. That competition drives prices down. In fact, when the first generic hits the market, prices typically drop 80% to 85% within the first year. With more manufacturers joining, prices fall even further.
By 2022, generic and biosimilar medications saved the U.S. healthcare system $408 billion. That’s up from $373 billion the year before. Over the past decade, those savings have totaled $2.9 trillion. Think about that: nearly $3 trillion saved because people chose a pill with a different name on the label.
Therapeutic Substitution: The Hidden Savings Most People Don’t Know About
Most people think savings come from swapping a brand-name drug for its generic. But there’s another layer: switching from one generic to another that’s cheaper but just as effective.
A 2022 study from Johns Hopkins looked at the top 1,000 generic drugs in Colorado. They found 45 high-cost generics that had lower-cost alternatives - meaning two different generics for the same condition, but one cost 15 times more than the other. For example, one version of a generic statin cost $120 a month, while another, equally effective version cost just $8. That’s a 93% discount.
These aren’t rare cases. In 62% of the high-cost generics studied, the cheaper alternative was just a different strength or dosage form of the same drug. Doctors and pharmacists can often switch patients to these lower-cost versions without changing the treatment plan. But most people don’t know this is even an option.
One pharmacist in San Diego told me he routinely asks patients: "Is this the cheapest generic we have for this condition?" He says 70% of the time, there’s a better option - and he can save them $50 to $200 a month.

Why Aren’t More People Using Generics?
Despite the savings, barriers still exist. One big one? Copays. Even when the wholesale price of a generic drops, some insurance plans don’t lower the patient’s copay. A 2023 AAM report found that many patients are still paying too much for generics because their insurance hasn’t updated their formulary.
Another issue is fear. Some patients worry that generics aren’t as strong, or that they cause more side effects. That’s especially true for drugs with a narrow therapeutic index - like levothyroxine (for thyroid conditions) or warfarin (a blood thinner). While the FDA says these generics are safe, some patients report feeling different after switching. That’s not always because the drug is different - sometimes it’s because the inactive ingredients (fillers, dyes) vary between manufacturers. For most people, it’s not a problem. But for those with sensitivities or complex conditions, switching should be done carefully and monitored.
Then there’s the problem of trust. A 2023 survey by the Medicare Rights Center found that 41% of Medicare beneficiaries still struggled to afford their meds - even though 91% of their prescriptions were generics. That tells us generics alone can’t fix broken pricing systems. The U.S. still pays 2.78 times more for drugs than other wealthy countries. Generics help, but they’re not a full solution.
How to Make Sure You’re Getting the Best Deal
If you’re on a prescription, here’s how to save money without risking your health:
- Ask your doctor: "Is there a generic version of this drug?" Even if it’s not on the prescription, they can write "dispense as written" if you need the brand.
- Ask your pharmacist: "Is there a cheaper generic alternative for this medication?" They have access to formularies and can often find a lower-cost version you didn’t know existed.
- Use tools like GoodRx or SingleCare. These apps compare prices at local pharmacies and often show prices lower than your copay.
- Check your insurance formulary. If your plan lists multiple generics, pick the one with the lowest tier. Sometimes the difference is $30 a month.
- For chronic conditions like high blood pressure or diabetes, ask if your doctor can switch you to a generic with a proven track record - like metformin, lisinopril, or atorvastatin.
One woman in San Diego switched from a $140-a-month brand-name antidepressant to a $7 generic - and didn’t notice any difference in how she felt. She said, "I used to skip doses because I couldn’t afford it. Now I take it every day. That’s the real savings."
What’s Next for Generic Medications?
The future looks bright - but not without challenges. In 2022, the FDA approved 831 new generic drugs, the second-highest number ever. That means more competition, more price drops, and more savings.
The Inflation Reduction Act, which caps Medicare Part D out-of-pocket costs at $2,000 a year starting in 2025, will likely push even more people toward generics. If you’re paying less out of pocket, you’re more likely to stick with your meds - and generics make that easier.
But threats remain. Drug shortages are rising - 78% of the 312 active shortages in September 2023 were for generic drugs. That’s because many generics are made overseas, and supply chains are fragile. Also, some brand-name companies file dozens of patents just to delay generic entry. The FTC found that brand manufacturers file an average of 17.5 patents per drug to block competition.
Still, the trend is clear. Generics aren’t a stopgap - they’re the most powerful tool we have to control drug costs. And for millions of Americans, they’re the difference between taking your medicine - or skipping it.
What You Can Do Today
You don’t need to wait for policy changes to save money. Start with your next prescription. Ask the questions. Compare prices. Don’t assume the brand is better. And don’t let a higher price tag fool you - the science says otherwise.
Generic medications are safe. They’re effective. And they’re saving the U.S. healthcare system hundreds of billions every year. If you’re not using them, you’re paying more than you have to - and you’re not alone. Millions are doing the same. The good news? It’s easy to change that.
Are generic medications as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for quality, strength, purity, and potency as brand-name drugs. They must prove they deliver the same amount of active ingredient into your bloodstream at the same rate. Over 98% of generics are rated "AB" - meaning they’re therapeutically equivalent. While rare cases of side effects from inactive ingredients exist, these are uncommon and usually manageable with a pharmacist’s help.
Why do some people feel different on generic medications?
Some people notice differences when switching to a generic, especially with drugs that have a narrow therapeutic index - like levothyroxine, warfarin, or certain seizure medications. This isn’t because the active ingredient is different, but because the fillers, dyes, or coatings can vary between manufacturers. These changes can affect how quickly the drug is absorbed. For most people, it’s not an issue. But if you feel different after switching, talk to your doctor or pharmacist. They can help determine if you need to stick with one brand or switch back.
Can I save money by switching between different generic versions of the same drug?
Absolutely. Many generic drugs have multiple manufacturers, and prices can vary dramatically. A 2022 study found that some high-cost generics were 15 times more expensive than other generics for the same condition. For example, one generic version of a statin cost $120 a month, while another cost just $8. Your pharmacist can check which version is cheapest and whether it’s safe to switch. Always ask - you could save $50 to $200 a month.
Why are generics so much cheaper if they’re the same drug?
Brand-name drug companies spend billions on research, clinical trials, and marketing. Once the patent expires, generic manufacturers don’t have to repeat those expensive steps. They just need to prove their version works the same way. That cuts development time from 10-15 years to 3-5 years and reduces costs by 80% or more. The savings come from competition - when multiple companies make the same drug, prices drop fast.
Does insurance always cover generics?
Most insurance plans strongly encourage or require generics. In fact, many plans have lower copays for generics - sometimes as low as $0 to $10. But some plans still charge high copays even when the generic’s wholesale price has dropped. If your copay seems high, ask your pharmacist if there’s a cheaper generic version available, or use a discount app like GoodRx. Sometimes the cash price is lower than your insurance copay.
Are biosimilars the same as generics?
Biosimilars are similar to generics, but for biologic drugs - complex medications made from living cells, like insulin or rheumatoid arthritis treatments. Unlike small-molecule generics, biosimilars can’t be exact copies because biologics are too complex. But they must show no clinically meaningful differences in safety or effectiveness. They’re still much cheaper than the original biologic - and their use is growing. As of 2023, 41 biosimilars have been approved by the FDA, with potential to save $50 billion annually by 2025.



Did you know that the FDA’s bioequivalence standards for generics allow for a 20% variance in absorption? That’s not a typo. It’s the legal loophole that lets companies slap a generic label on a pill that might hit your bloodstream slower-or faster-than the brand. I’ve seen people switch to generics and end up in the ER because their seizure meds didn’t kick in on time. Science? Sure. But science doesn’t care if you’re the one paying the price.
So let me get this straight-we’re celebrating generics like they’re some kind of miracle cure, but the real problem is that drug companies are charging $450 for a pill that costs 7 cents to make? Yeah, I’m not mad, I’m just disappointed. And the fact that we’re still talking about this in 2025? Classic America.
My mom switched from brand-name Zoloft to generic sertraline and saved $420 a month. She didn’t feel any different-same mood, same sleep, same ability to not cry during commercials. If you’re still paying full price because you think the brand is ‘better,’ you’re not being careful-you’re being exploited. Ask your pharmacist. Use GoodRx. Don’t let greed decide your health.
But what if the generic makes you feel like a zombie? I switched and my brain just… stopped. Like my thoughts were underwater. I went back to the brand and I’m alive again. Who’s to say it’s not the fillers? They could be poisoning us slowly.
Generics are a government scam. The FDA is owned by Big Pharma. That’s why they approve 98% of them. They want you to think you’re saving money so you don’t ask why insulin still costs $300. The real drug companies? They’re laughing all the way to the Swiss bank. Wake up.
Just checked GoodRx-my generic lisinopril is $3 at Walmart but $18 at CVS. 😳 I’m switching tomorrow. Why didn’t anyone tell me this sooner?? 🤯
One thing people overlook: switching between generic manufacturers can matter more than brand vs. generic. I’m a pharmacist and I’ve seen patients stabilized on one generic version of levothyroxine, then switched to another because of insurance, and their TSH went haywire. It’s not the active ingredient-it’s the formulation. Always ask your doctor to specify ‘dispense as written’ if you’re sensitive. Small changes, big effects.
They say generics are 90% of prescriptions but only 1.5% of spending. That math doesn’t add up unless you’re ignoring the fact that 40% of people still skip doses because they can’t afford the copay-even on generics. The system isn’t broken, it’s designed to make you feel like you’re winning while they win bigger.
Yeah but what about the 2% of generics that aren’t AB rated? You think that’s negligible? That’s still thousands of people a year having bad reactions. And nobody tracks it. The FDA doesn’t require post-market studies for generics. So if you’re one of those people, you’re just… out of luck.