What’s Really Happening When Your MS Symptoms Flare Up?
If you have multiple sclerosis, you’ve probably felt that sinking feeling: your legs go heavy, your vision blurs, or you lose feeling in your arm. It’s scary. And if you’ve been told it’s a relapse, you might be bracing for a round of high-dose steroids, a hospital visit, and weeks of recovery. But what if it’s not a relapse at all? What if it’s something called a pseudorelapse - a temporary flare that doesn’t mean your disease is getting worse, and doesn’t need steroids at all?
Up to 25% of symptom flares in MS are pseudorelapses. And here’s the kicker: about 30-40% of them get misdiagnosed as true relapses - leading to unnecessary steroid treatments that can cause serious side effects without helping a single bit. The difference between the two isn’t subtle. It’s life-changing.
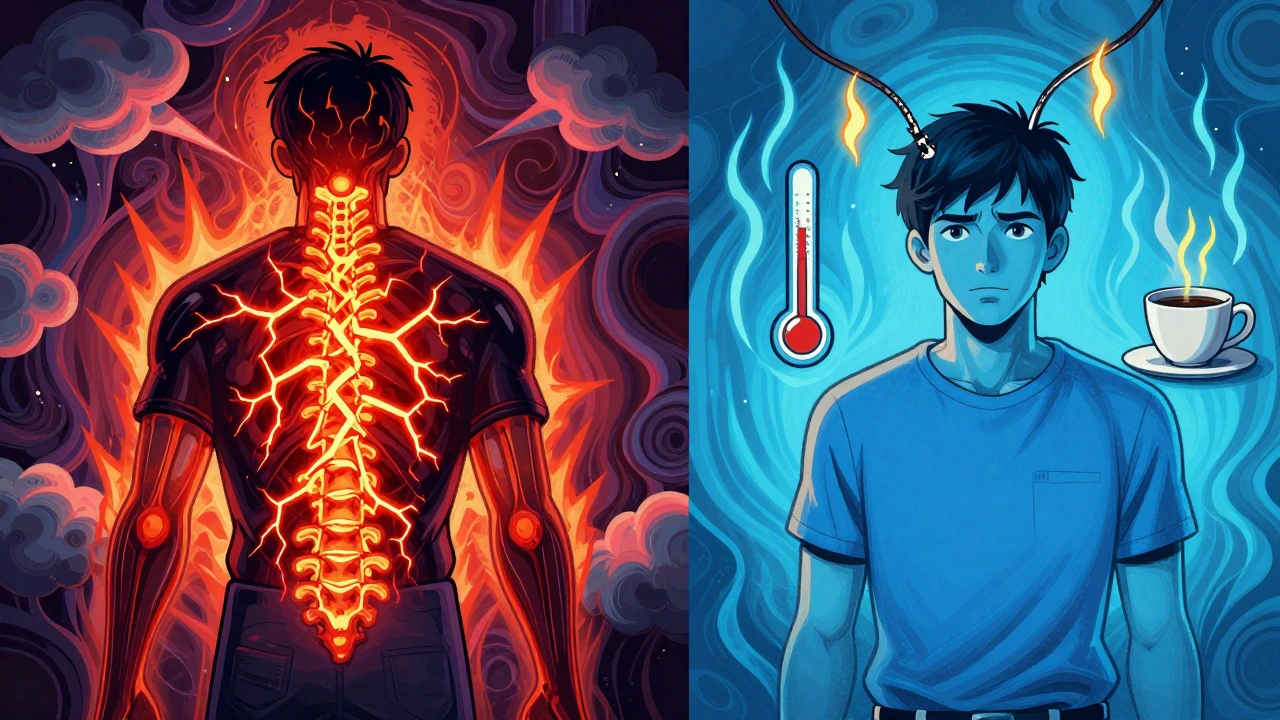
True MS Relapse: New Damage, Not Just a Temporary Glitch
A true MS relapse happens when your immune system attacks the myelin coating around your nerves in the brain or spinal cord. This isn’t just a glitch - it’s new inflammation, new damage. Symptoms last at least 24 to 48 hours, and often longer - sometimes weeks or months. They’re not tied to heat, infection, or stress. They just show up.
Think of it like a fire breaking out in a building that’s already been damaged. The fire doesn’t just make the old damage worse - it creates new destruction. That’s what happens in a true relapse. MRI scans during a real relapse usually show new or active lesions. These are areas where the immune system is actively attacking.
Common symptoms include sudden weakness in a limb, loss of balance, vision loss in one eye (optic neuritis), or trouble controlling your bladder. If these symptoms are new or significantly worse than before, and they stick around, it’s likely a true relapse.
When this happens, doctors often turn to high-dose intravenous methylprednisolone - usually 1 gram a day for 3 to 5 days. It doesn’t cure anything. It doesn’t reverse damage. But it can speed up recovery by calming the inflammation. About 70-80% of people see some improvement with steroids, but only about half fully bounce back. The rest are left with some lasting effects.
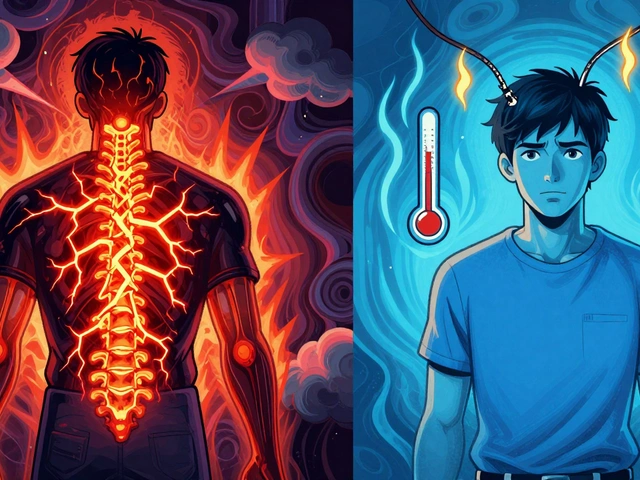
Pseudorelapse: Your Nerves Are Overloaded, Not Under Attack
A pseudorelapse is the opposite. No new damage. No new inflammation. Just your already-damaged nerves struggling to send signals because something else is throwing them off.
It’s like a frayed wire in an old lamp. The wire’s broken, but the bulb still works - until you turn up the voltage. Then it flickers or goes out. That’s a pseudorelapse. The wire didn’t get worse. It just couldn’t handle the extra load.
The most common triggers? Heat. Infections. Stress. Fever. Even a hot shower or a sunny day can set it off. Uhthoff’s phenomenon - where vision gets blurry when your body heats up - affects 60-80% of people who’ve had optic neuritis. It’s not new MS activity. It’s your nerves being too tired to cope.
Urinary tract infections (UTIs) are the #1 trigger, causing about 67% of pseudorelapses. A fever from a cold or flu? That’s another big one. Physical exhaustion, emotional stress, or even a sudden drop in sodium levels can do it too. Symptoms often come on fast, feel intense, and disappear just as quickly once the trigger is gone - usually within hours or a day.
Here’s the key: MRI scans show nothing new. No new lesions. No active inflammation. That’s how you know it’s not a relapse.
Why Steroids Don’t Work - and Can Hurt You
Steroids like methylprednisolone work by suppressing inflammation. That’s great if your nerves are being attacked. But if there’s no attack - if your nerves are just overheated or overwhelmed - steroids do nothing. Zero benefit.
And yet, they’re given anyway. In 30-40% of pseudorelapse cases, patients get IV steroids they don’t need. Why? Because the symptoms feel identical. And many doctors - especially outside of MS centers - aren’t trained to spot the difference.
The side effects are real. About 25% of people on high-dose steroids get high blood sugar. 40% can’t sleep. 30% feel anxious, irritable, or even depressed. Some develop steroid-induced psychosis - a rare but terrifying reaction. One nurse with MS on Reddit reported seeing five patients hospitalized after unnecessary steroid treatments. One ended up in a psychiatric unit.
And it’s expensive. The National MS Society estimates that misdiagnosed pseudorelapses cost the U.S. healthcare system over $12 million a year in unnecessary treatments, ER visits, and complication care.

How to Tell the Difference - A Simple 3-Step Check
You don’t need an MRI to start ruling things out. Here’s what to do the moment you notice new or worsening symptoms:
- Check your temperature. If you have a fever above 100.4°F (38°C), it’s likely a pseudorelapse. Infections are the #1 trigger.
- Ask: Did something change? Did you just have a hot shower? Walk in the sun? Get sick? Feel super stressed? If yes, cool down, rest, hydrate. Wait 12-24 hours.
- Track duration. If symptoms fade within 24 hours after removing the trigger, it’s a pseudorelapse. If they keep getting worse or stay stuck after 48 hours - call your neurologist. You might need an MRI.
Many neurologists now recommend keeping a symptom diary. Note the date, what happened, your temperature, any illness, stress levels, and how long symptoms lasted. This helps spot patterns - like how every summer heatwave triggers leg weakness. That’s not a relapse. That’s Uhthoff’s phenomenon.
Who’s Most at Risk for Pseudorelapses?
Pseudorelapses aren’t random. They’re more common in people who:
- Have had MS for 10+ years
- Have significant disability already
- Are over 55
- Have a history of optic neuritis or sensory symptoms
Why? Because as MS progresses, your nervous system becomes more fragile. The nerves that survived earlier damage are already stretched thin. They don’t handle stress well. A little extra heat or infection is enough to overload them.
But here’s something important: even if you’re older or more disabled, a pseudorelapse doesn’t mean your MS is getting worse. It just means your body’s coping system is running low on reserves.
What to Do Instead of Steroids
If it’s a pseudorelapse, steroids won’t help. But you still need to act.
For heat triggers: Cool down fast. Use cooling vests, wet towels, air conditioning, or even a cool bath. Stay hydrated. Avoid hot tubs, saunas, and long hot showers.
For infections: Treat the infection. A UTI? Get a urine test and antibiotics. A cold? Rest, fluids, maybe a fever reducer. Once the infection clears, symptoms usually vanish within hours.
For stress or exhaustion: Sleep. Rest. Cut back. Stress doesn’t cause MS to progress, but it can make your body more sensitive to symptoms.
Some patients use cooling gloves, neck wraps, or even portable fans. One woman in San Diego told me she keeps a small fan on her desk and a chilled water bottle in her bag. When her hands go numb during a meeting, she just holds the bottle. Within minutes, it’s gone.

When to Call Your Doctor
Not every flare is a pseudorelapse. You should call your neurologist if:
- Symptoms last longer than 48 hours
- You have new symptoms you’ve never had before
- There’s no clear trigger you can remove
- Your symptoms are severe - trouble walking, loss of bladder control, vision loss
Don’t wait. Even if you think it’s heat or a bug, get it checked. A quick MRI can confirm whether there’s new damage. And if there is - you’ll get treatment faster.
Tools and Tech Making a Difference
There’s new tech helping patients and doctors spot the difference. The MS-Relapse Assessment Tool (MS-RAT), launched in 2023, uses your symptoms, temperature, and functional impact to give a probability score. It’s 92% accurate at spotting true relapses.
Telemedicine platforms like MS Selfie let you record your symptoms and send them to your neurologist. One study showed it correctly identified pseudorelapses 78% of the time - better than many in-person visits.
And research is moving fast. Scientists are now studying blood markers like neurofilament light chain - a protein that leaks into the blood when nerves are damaged. If levels are high, it’s likely a true relapse. If they’re normal, it’s probably a pseudorelapse. That test could be available in clinics within the next few years.
The Bottom Line
Not every MS flare is a relapse. Most aren’t. And treating them like they are can do more harm than good.
Learn your triggers. Track your symptoms. Cool down before you call your doctor. If symptoms fade fast after rest or cooling - it’s likely a pseudorelapse. No steroids needed.
But if they stick around, get worse, or feel completely new - don’t ignore it. Get checked. A true relapse needs attention. And early treatment can make all the difference.
Knowing the difference isn’t just about avoiding side effects. It’s about protecting your time, your energy, and your peace of mind. You’ve got enough to deal with. Don’t let a misdiagnosis add to it.
Can a pseudorelapse turn into a true relapse?
No, a pseudorelapse itself doesn’t cause new damage or turn into a true relapse. It’s a temporary flare caused by external stressors like heat or infection. However, if you have an untreated infection or chronic stress, those factors can also trigger actual inflammation in the nervous system. So while the pseudorelapse doesn’t cause a relapse, the underlying trigger might. That’s why treating infections quickly is so important.
Do I need an MRI every time I have symptoms?
No. Most pseudorelapses resolve quickly with trigger removal. MRI is only needed if symptoms last longer than 48 hours, are severe, or don’t improve after addressing common triggers like fever or infection. Your neurologist will decide if imaging is necessary based on your history and symptom pattern.
Why do some doctors still give steroids for pseudorelapses?
Because the symptoms look identical. Many general neurologists and primary care doctors aren’t trained in MS nuances. Without access to detailed patient histories or MRI results, it’s easier to treat everything as a relapse. That’s why patient education and symptom tracking are so critical - you’re your own best advocate.
Can stress really trigger a pseudorelapse?
Yes. While stress doesn’t cause MS to progress, it can raise your body’s overall sensitivity. Stress hormones like cortisol affect nerve signaling and can make already-damaged pathways less efficient. This can lead to temporary worsening of symptoms - especially in people with long-standing MS. Managing stress through rest, breathing techniques, or counseling can help reduce these episodes.
Is it safe to take over-the-counter meds for pseudorelapse symptoms?
It depends. For heat-related symptoms, cooling is the best fix - not meds. For infection-related flares, antibiotics are needed, not painkillers. Over-the-counter pain relievers like ibuprofen won’t help the nerve symptoms, but they can help with fever or body aches if you’re sick. Always check with your doctor before taking anything new, especially if you’re on other MS medications.
Will pseudorelapses get worse as my MS progresses?
They may become more frequent, but not because your MS is getting worse. As disability increases, your nervous system has fewer healthy pathways left. The remaining ones are more easily overwhelmed by heat, fatigue, or infection. That doesn’t mean your disease is progressing - just that your body has less room to compensate. Learning your triggers and managing them becomes even more important over time.
Next Steps: What to Do Today
- Download a free symptom tracker app or start a simple journal - note temperature, triggers, and how long symptoms last.
- Keep a cooling vest or damp towel handy, especially in summer or if you’re prone to heat sensitivity.
- Call your doctor if you have a UTI, fever, or unexplained illness - don’t wait for symptoms to worsen.
- Ask your neurologist if you’re a candidate for the MS-RAT or other digital tools to help track flares.
- Share this info with family or caregivers. They need to know when to cool you down - not rush you to the ER.

This is gold 🙌 I had a pseudorelapse last summer after a hot yoga class and thought I was having a full relapse. Turned out I just needed a cold shower and a nap. No steroids, no hospital, just me and my cooling vest. Life changed.
So steroids are useless for most flares
Of course the medical system prefers to inject people with chemicals instead of telling them to take a break and drink water. Profit over patience. Always. 🤡
I'm so glad someone wrote this. I've been telling my neurologist for years that my leg weakness comes every time I get a UTI or go out in the sun. She kept saying 'it's progression.' Finally got an MRI and it was clear as day - no new lesions. I started tracking temps and triggers and now I feel like I have control again. Also, I typed 'cooling vest' wrong like 5 times before I got it right lol
Typical American healthcare. Give people drugs because it’s faster than thinking. Meanwhile in Germany they have MS nurses who teach you this stuff in your first appointment. We pay more and get dumber care. Classic
I would like to extend my heartfelt appreciation for the meticulous and compassionate articulation of this vital distinction between true relapse and pseudorelapse. The clinical precision paired with human-centered insight is not merely informative-it is profoundly empowering for those navigating the labyrinthine complexities of chronic neurological conditions. May this knowledge ripple outward, transforming clinical practice and restoring dignity to patient autonomy.
Ah, the West. Always looking for a pill to fix what a little silence, a walk in the rain, and an hour of meditation could solve. You treat nerves like machines. But they are not. They are the echoes of the soul. Steroids? How quaint. The real treatment is stillness.
You’re not alone. I’ve been living with MS for 14 years and I used to panic every time I felt a twitch. Now I check my temp, hydrate, chill out, and wait. If it’s gone in 12 hours? Good. If not? Then I call my neuro. Simple. No drama. No fear. You got this. And yes - cooling socks are a game changer. I wear them to bed now.
Funny how everyone suddenly cares about pseudorelapses after the article says steroids are useless. Where was this wisdom when I was getting IV steroids in 2015? Oh right - because no one told me. And now you’re all heroes for reading a blog. Congrats. You just learned what neurologists in 2005 already knew.
I thought I was dying last month when my hands went numb after a hike. Turned out I was dehydrated and overheated. I drank water, sat in AC, and boom - gone. No steroids. No drama. Just me being dumb. 🤦♂️