Antiviral mechanism: how antiviral drugs stop viruses
Viruses hijack cells to make more copies of themselves. Antiviral mechanisms are the specific ways drugs interrupt that process. Knowing how a medicine works helps you understand why timing, dosing, and drug choice matter.
Major antiviral targets
Entry inhibitors block the virus from getting into a cell. Some drugs and monoclonal antibodies bind viral surface proteins or cell receptors. Examples: maraviroc blocks HIV's CCR5 co-receptor, and monoclonal antibodies can neutralize viruses like RSV or SARS-CoV-2.
Uncoating inhibitors stop the virus from shedding its protective coat once inside. Older flu drugs like amantadine targeted this step, but many viruses quickly develop resistance, so these drugs are rarely used now.
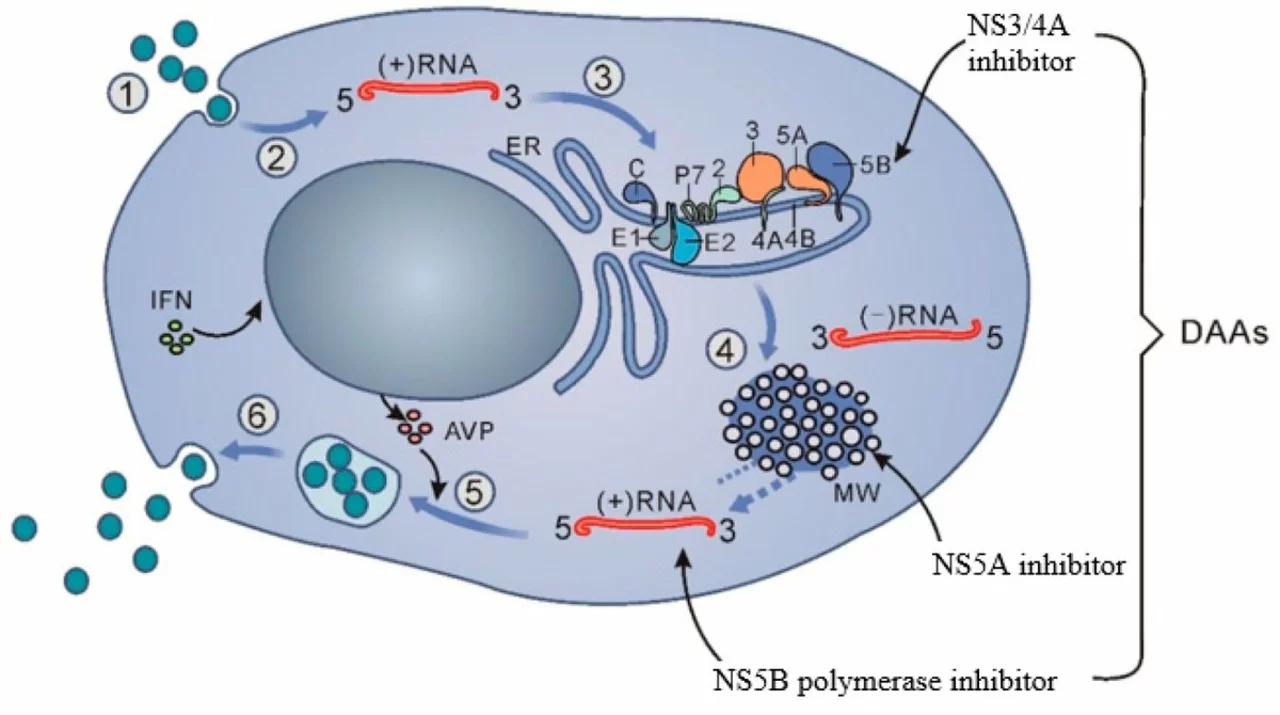
Polymerase inhibitors and nucleoside/nucleotide analogs target viral genome copying. These mimic the building blocks of RNA or DNA and cause chain termination or faulty copies. Acyclovir (for herpes) and sofosbuvir (for hepatitis C) are classic examples; remdesivir is an example used against some RNA viruses.
Protease inhibitors prevent viral proteins from being cut into usable pieces. Viruses like HIV and hepatitis C need protease enzymes to assemble infectious particles. Drugs such as lopinavir/ritonavir or glecaprevir block that enzyme and leave immature, noninfectious particles behind.
Assembly and release inhibitors stop the final steps: putting together virus parts or leaving the cell. Oseltamivir targets influenza neuraminidase to slow release; baloxavir blocks a viral endonuclease needed for flu virus replication—both limit spread in the body.
Host-targeted antivirals act on cell functions the virus needs. Interferons boost innate defenses; other drugs may inhibit host enzymes that viruses exploit. These can reduce resistance risk but sometimes cause more side effects because they affect human cells.
What this means for you
Start antiviral treatment early when possible. Many antivirals work best if given within days of symptoms because they stop replication, not damage already done. Missing doses or stopping early raises the chance of resistance.
Watch for drug interactions and side effects. Protease inhibitors, for example, interact with common heart and cholesterol meds via CYP3A4. Always tell your prescriber about other drugs and supplements.
Antivirals aren’t antibiotics. They won’t help bacterial infections. For many viruses, prevention (vaccines, masks, hand hygiene) is still the best strategy. When antivirals are available, doctors pick them based on the virus, illness stage, and patient health.
Research keeps moving toward broad-spectrum drugs, better oral antivirals, and tailored monoclonal antibodies. If you have questions about a specific antiviral, ask your healthcare provider for details about how it works, timing, and safety for your situation.
As a blogger, I've been researching the science behind Daclatasvir and how it works. From what I've discovered, this powerful antiviral drug is specifically designed to treat Hepatitis C by inhibiting the replication of the virus. Daclatasvir targets a protein called NS5A, which plays a crucial role in the virus's life cycle. By blocking this protein, Daclatasvir disrupts the ability of the virus to multiply and, ultimately, helps to clear it from the body. I find it fascinating how this medication can provide such a targeted and effective treatment for those suffering from Hepatitis C!