MS Relapse: What It Is, How It Happens, and What You Can Do
When you have MS relapse, a sudden return or worsening of multiple sclerosis symptoms lasting more than 24 hours, with no other cause like infection or heat exposure. Also known as a MS flare-up, it’s not just feeling tired—it’s your nervous system sending out distress signals. This isn’t a new diagnosis. It’s your existing condition pushing through a temporary breakdown in control. About 85% of people with multiple sclerosis start with relapsing-remitting MS, where these episodes come and go, often without warning.
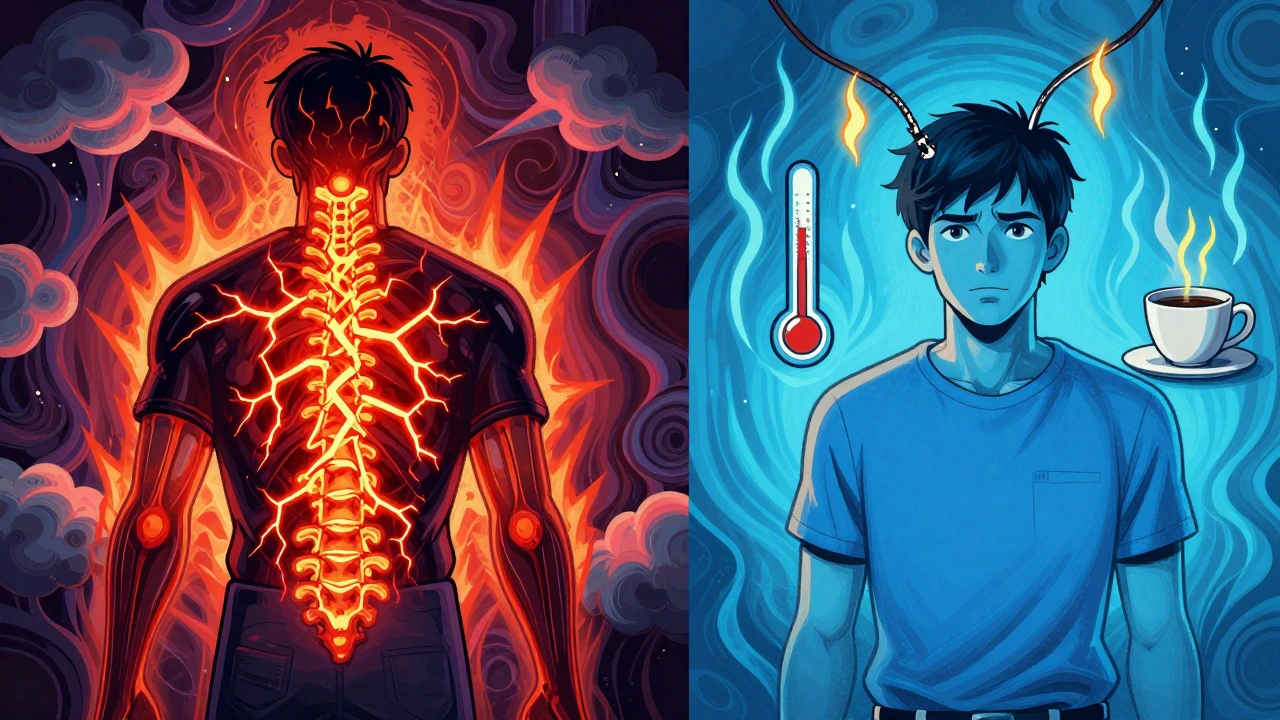
What causes an MS relapse? It’s not stress alone, though that can play a role. The real trigger is immune activity—your body’s own defense system mistakenly attacks the protective coating around your nerve fibers, called myelin. This damage slows or blocks signals between your brain and body. That’s why you might suddenly lose balance, feel numbness, or struggle to walk. These aren’t random. They’re direct results of inflammation in your central nervous system. Disease-modifying therapies, medications designed to reduce the frequency and severity of MS relapses by calming the immune system are the backbone of long-term management. Drugs like interferons, ocrelizumab, or fingolimod don’t cure MS, but they cut down how often these flare-ups hit—and how bad they get.
Not every spike in symptoms is a true relapse. Sometimes, a fever, hot shower, or even a stressful day can make you feel worse temporarily. That’s called a pseudo-relapse. It’s scary, but it’s not new damage. Your nerves are just extra sensitive right now. The key difference? A real relapse lasts over 24 hours and shows up on an MRI as new lesions. A pseudo-relapse fades when the trigger goes away. Knowing this saves you from panic—and unnecessary steroid treatments.
When a real relapse happens, doctors often turn to high-dose corticosteroids, powerful anti-inflammatory drugs given intravenously to shorten the episode and speed recovery. They don’t change the long-term course of MS, but they can get you back on your feet faster. Some people recover fully. Others are left with lingering effects. That’s why tracking symptoms over time matters. Keep a journal. Note when things got worse, what you were doing, and how long it lasted. That info helps your neurologist decide if your treatment plan needs tweaking.
There’s no magic bullet to stop every relapse, but you’re not powerless. Staying out of extreme heat, managing infections fast, and sticking to your meds are the biggest things you can control. Exercise, sleep, and reducing stress won’t cure MS, but they help your body handle the pressure. And if you’ve had more than two relapses in a year, or your symptoms are getting worse between episodes, it’s time to talk about switching therapies. Your current drug might not be cutting it anymore.
Below, you’ll find real, practical guides on managing MS symptoms, understanding your meds, spotting early warning signs, and avoiding common mistakes that make relapses worse. No fluff. Just what works—based on clinical data and patient experience.
Learn how to tell the difference between a true MS relapse and a pseudorelapse - and why steroids aren’t always the answer. Discover triggers, symptoms, and what to do instead.