Pseudorelapse: What It Is and How It Affects Chronic Disease Management
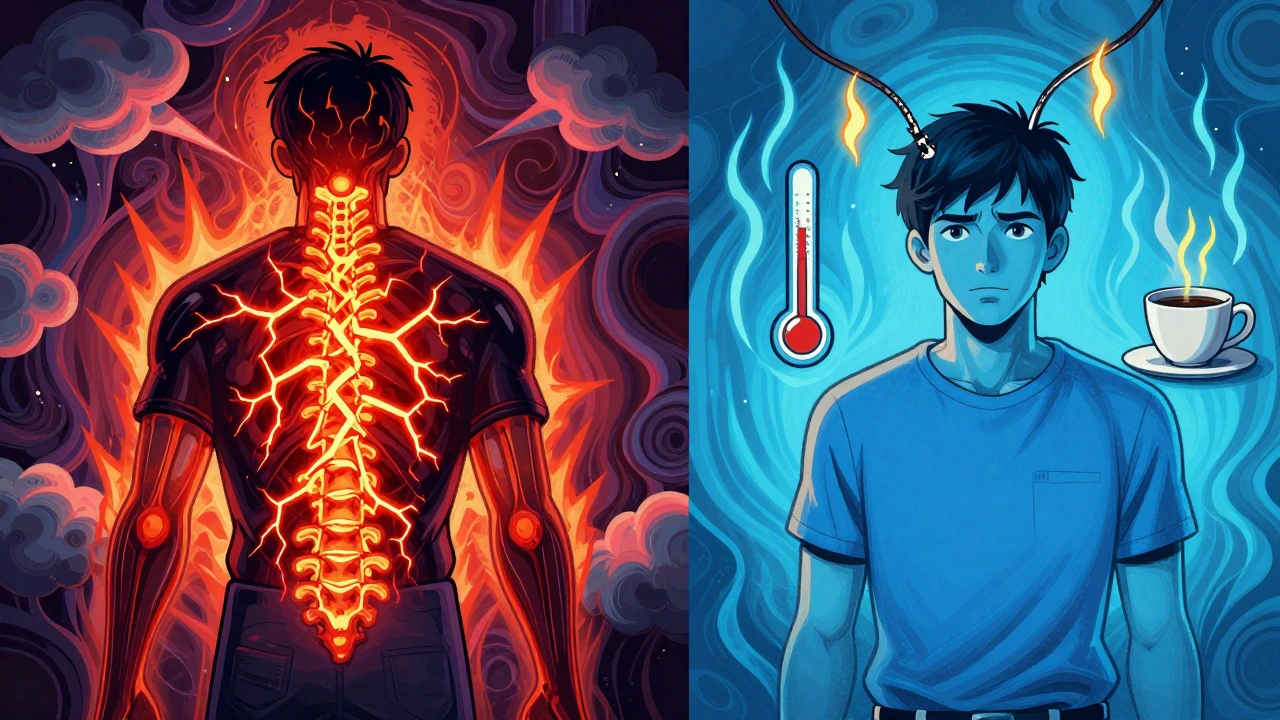
When your symptoms come back but your disease hasn’t actually worsened, you’re not having a relapse—you’re experiencing a pseudorelapse, a temporary worsening of symptoms that mimics disease progression but isn’t caused by the disease itself. Also known as a false flare, it’s a common trap for people managing chronic conditions like multiple sclerosis, lupus, or inflammatory bowel disease. You might feel worse, your doctor might see new signs, and your tests might look concerning—but the root cause isn’t your illness getting stronger. It’s something else entirely.
Pseudorelapse often gets confused with treatment failure, but the two are very different. A true relapse means your disease is actively attacking your body again. A pseudorelapse? That’s your body reacting to stress, infection, heat, sleep loss, or even a missed dose of medication. For example, someone with multiple sclerosis might have a spike in fatigue and numbness after a bad night’s sleep or a cold—not because their MS is progressing, but because their nervous system is already on edge. The same thing happens with lupus patients after a viral infection, or with IBD patients who skip their anti-inflammatory meds for a few days. The symptoms look real, but the trigger isn’t the disease. It’s the medication adherence, the consistent use of prescribed drugs at the right time and dose. Missed doses, wrong timing, or even switching brands can throw off your body’s balance and create the illusion of worsening illness.
Another big player in pseudorelapse is treatment resistance, when a therapy stops working as well as it once did, not because the disease changed, but because your body adapted. Think of it like a phone battery that drains faster after years of use—the battery isn’t broken, it’s just worn out. Some medications lose effectiveness over time due to changes in how your body absorbs them or how your immune system responds. That doesn’t mean you need stronger drugs—it might mean you need a different schedule, a different formulation, or even just a break. And that’s where pseudorelapse gets dangerous: if you assume it’s a real flare, you might end up on stronger, riskier treatments you don’t need. But if you ignore it, you might miss something real, like an infection or a new complication.
What you need to do when symptoms return isn’t panic—it’s track. Write down what changed in the days before the flare: Did you get sick? Skip a pill? Travel? Sleep less? Drink more caffeine? Stress more? These aren’t just background details—they’re clues. Doctors use this info to separate pseudorelapse from true progression. And if you’re the one managing your condition, knowing the difference gives you power. You can adjust your habits instead of your meds. You can rest instead of rush to the ER. You can talk to your doctor with facts, not fear.
Below, you’ll find real-world stories and science-backed guides on how to spot pseudorelapse, avoid common mistakes, and work with your treatment plan so you’re not chasing ghosts—while still being ready for the real threats.
Learn how to tell the difference between a true MS relapse and a pseudorelapse - and why steroids aren’t always the answer. Discover triggers, symptoms, and what to do instead.