Steroid Use MS: What You Need to Know About Safety, Risks, and Alternatives
When someone with multiple sclerosis, a chronic autoimmune disease that affects the central nervous system. Also known as MS, it experiences a flare-up—like sudden weakness, vision loss, or numbness—doctors often turn to corticosteroids, powerful anti-inflammatory drugs used to reduce swelling in the nerves. These aren’t cures. They don’t stop MS from progressing. But they can shorten the worst of a relapse, helping people get back on their feet faster. That’s why steroid use in MS is common, but also misunderstood.
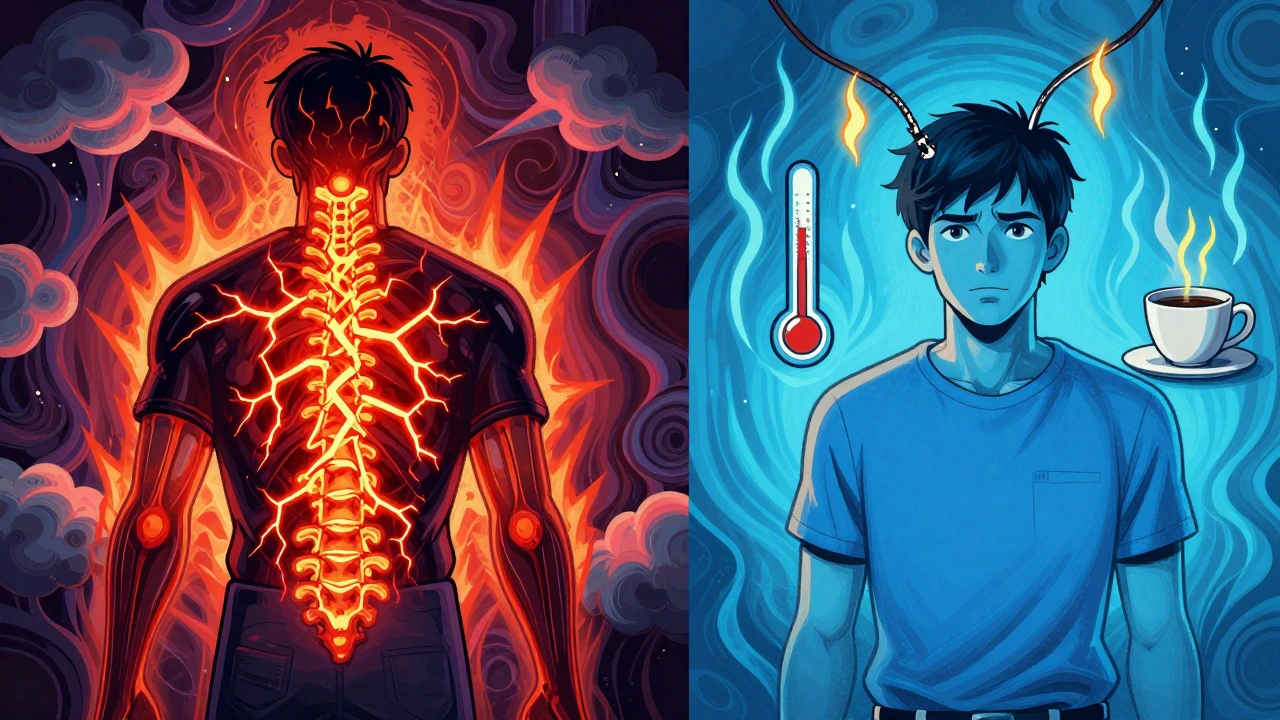
Most people get a short course of high-dose steroids, usually prednisone or methylprednisolone, a synthetic steroid often given intravenously during MS attacks, over 3 to 5 days. It works by calming the immune system’s attack on nerve coverings. But it’s not harmless. Side effects like insomnia, mood swings, stomach upset, and elevated blood sugar are normal. For some, it triggers anxiety or even panic attacks. Long-term use? That’s where things get dangerous: bone thinning, muscle loss, increased infection risk, and adrenal suppression. That’s why doctors don’t prescribe steroids for daily MS control—they’re emergency tools, not maintenance drugs.
Many people assume steroids are the best or only option during an MS flare. But that’s not true. Some relapses fade on their own. Others respond better to plasma exchange if steroids don’t work. And newer disease-modifying therapies like ocrelizumab or fingolimod can reduce how often flares happen in the first place. If you’re on steroids often, it might mean your long-term treatment isn’t working well enough. That’s a signal to talk to your neurologist—not just to get more steroids, but to rethink your overall plan.
What you won’t find in most doctor’s offices is honest talk about what steroids really do to your body. They mask symptoms. They don’t fix the problem. And if you’re using them repeatedly because you’re afraid of what happens without them, you’re not alone. But you don’t have to stay stuck there. The posts below cover real cases: how one person managed MS without daily steroids, why some people develop steroid-induced diabetes, what alternatives actually work, and how to tell if your flare needs a steroid—or just rest and time.
Learn how to tell the difference between a true MS relapse and a pseudorelapse - and why steroids aren’t always the answer. Discover triggers, symptoms, and what to do instead.