
Child Antihistamine Dosing Calculator
How to Use This Calculator
Enter your child's information below. This tool calculates safe antihistamine doses based on guidelines from Boston Children's Hospital and the American Academy of Allergy, Asthma & Immunology.
- Weight: Always use exact weight (in kg or lbs) - don't guess!
- Measurement: Use the measuring device that came with the medicine - never a kitchen spoon.
- Age: Some medications have specific age restrictions (e.g., Zyrtec approved for infants 6+ months).
When your child breaks out in hives after eating peanuts, or their nose won’t stop running during pollen season, it’s tempting to reach for an antihistamine. But giving your child medicine meant for adults can be dangerous - and not all antihistamines are created equal. The right choice depends on age, weight, and the type of reaction. For kids, it’s not just about stopping the itch - it’s about avoiding side effects that can be serious, even life-threatening.
Why Age Matters More Than You Think
Children aren’t small adults. Their bodies process medicine differently. A baby’s liver and kidneys aren’t fully developed, so drugs like diphenhydramine (Benadryl) can build up in their system and cause extreme drowsiness, confusion, or even breathing problems. That’s why the FDA warns against using Benadryl in children under 2 years old without a doctor’s order. Even for kids older than 2, the risks don’t disappear.Second-generation antihistamines like cetirizine (Zyrtec) and loratadine (Claritin) are now the standard for most pediatric allergies. Why? Because they don’t cross the blood-brain barrier as easily. That means less drowsiness, less dry mouth, and fewer chances of confusion or rapid heartbeat. A 2020 study in Pediatric Allergy and Immunology found that only 10-15% of children on cetirizine felt sleepy, compared to 50-60% on diphenhydramine. That’s a huge difference when your child needs to go to school or play outside.
Dosing by Age: Exact Numbers You Can Trust
There’s no one-size-fits-all dose. It’s not about how old your child looks - it’s about their weight and the specific medicine. Here’s what current guidelines from Boston Children’s Hospital, Children’s Hospital Colorado, and the American Academy of Allergy, Asthma & Immunology recommend:
- Infants 6 to 11 months: Cetirizine at 0.25 mg per kg of body weight per day (e.g., 2.5 mg for a 10 kg baby). Some doctors start lower - at 0.125 mg/kg - especially if symptoms are mild. This is off-label use, but backed by research and recommended by pediatric allergists.
- Children 1 to 2 years: Cetirizine 2.5 mg daily (½ teaspoon of liquid, 5 mg/5 mL). Loratadine is not FDA-approved for this age group, so use only if prescribed.
- Children 2 to 5 years: Cetirizine 2.5 mg to 5 mg daily. Loratadine 5 mg daily (1 teaspoon of liquid or one 5 mg tablet). Do not use chewables unless you confirm each tablet is exactly 5 mg - some are 10 mg.
- Children 6 to 11 years: Cetirizine 5 to 10 mg daily. Loratadine 10 mg daily. You can split the dose if needed (e.g., 5 mg twice a day for cetirizine).
- Children 12 and older: 10 mg of cetirizine or loratadine once daily.
For diphenhydramine (Benadryl), use only under a doctor’s direction. If prescribed:
- Children 38-49 lbs: 7.5 mL of liquid (12.5 mg) every 6 hours, max 6 doses in 24 hours.
- Children 50-99 lbs: 10 mL (15 mg) every 6 hours, max 6 doses.
Never guess. Always check the label. A common mistake? Using adult Zyrtec tablets (10 mg) for a 4-year-old. That’s double the safe dose.
Measurement Matters: Why Your Kitchen Spoon Is Dangerous
One of the most dangerous mistakes parents make is using a regular teaspoon to measure liquid medicine. A kitchen spoon holds anywhere from 3 mL to 7 mL - that’s a 50% error. Boston Children’s Hospital found that nearly 40% of parents give the wrong dose because they use kitchen utensils.
Always use the measuring cup, syringe, or dropper that came with the bottle. If it’s missing, ask your pharmacy for a new one. They’ll give you a free, accurate tool. Never assume that the cap or a juice cap is the right size. If the medicine says “5 mg per 5 mL,” and you give 7 mL, you’ve given 7 mg - way too much for a toddler.
First-Generation vs. Second-Generation: What’s the Real Difference?
There are two big groups of antihistamines. The first-generation - like diphenhydramine (Benadryl), chlorpheniramine, and hydroxyzine - are older. They work fast, but they hit the brain hard. That’s why they’re used for sleep or motion sickness in adults. But in kids, they cause more harm than good.
Second-generation - cetirizine, loratadine, fexofenadine - are designed to stay out of the brain. They last longer, need fewer doses, and have far fewer side effects. Cetirizine is the most studied in young children. It’s approved for babies as young as 6 months. Loratadine is approved for kids 2 and up. Both are safe for daily use in chronic allergies like eczema or hay fever.
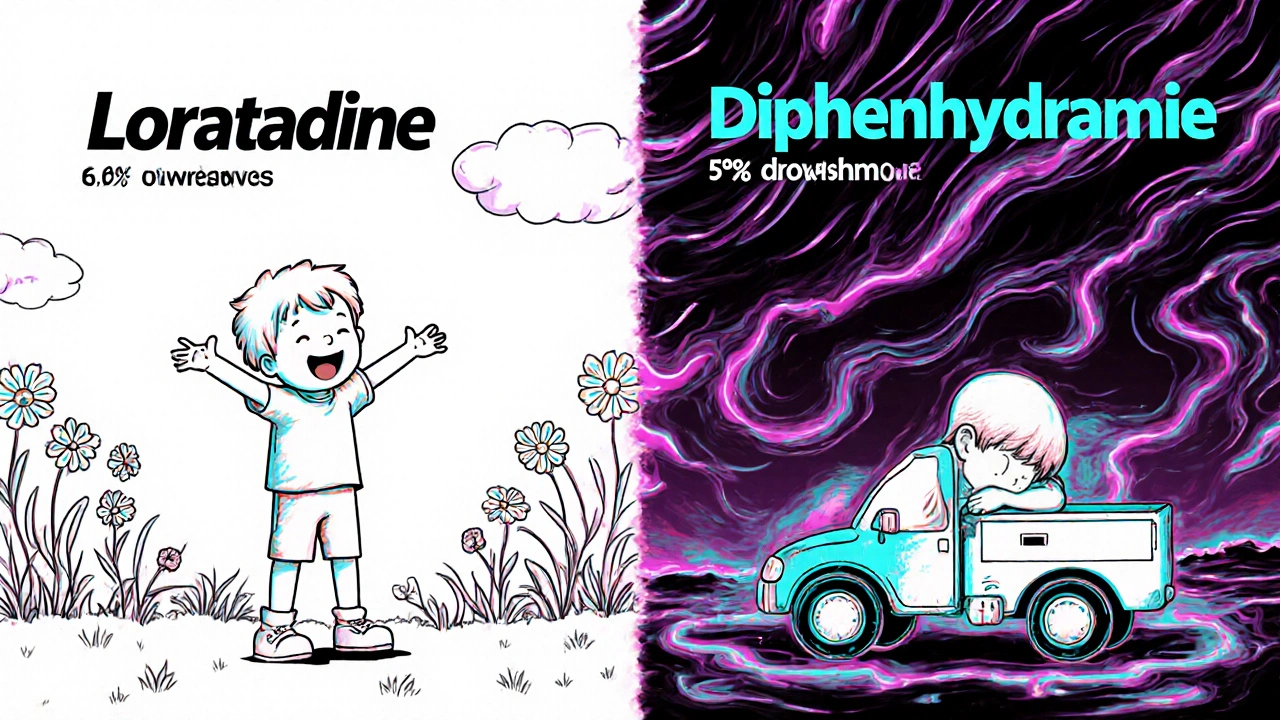
Here’s the catch: cetirizine causes slightly more drowsiness than loratadine. One study showed 14.7% of kids on cetirizine felt sleepy, compared to 6.9% on loratadine. If your child is already tired or has trouble sleeping, loratadine might be the better pick. But if you need strong, fast relief for hives or allergic swelling, cetirizine is still the top choice.
When to Avoid Antihistamines Altogether
Don’t use antihistamines to make your child sleepy. That’s not what they’re for. The American College of Allergy, Asthma, and Immunology says this practice triples the risk of overdose in kids under 2. One parent gave Benadryl to help their 18-month-old nap. The child became unresponsive, had dilated pupils, and needed emergency care. That’s not rare. Poison control centers see dozens of these cases every year.
Also, avoid combination products. Many cold and allergy medicines for kids include antihistamines plus decongestants, cough suppressants, or fever reducers. The FDA says these are not safe for children under 6. Why? Because you can’t control the dose of each ingredient. One medicine might have 12.5 mg of diphenhydramine and 10 mg of pseudoephedrine - too much for a small body.
And never use adult antihistamines for children. Even if you cut a tablet in half, the dose won’t be accurate. Tablets are made to be swallowed whole. Cutting them changes how they dissolve. Liquid is always safer for kids under 6.
What to Do in an Emergency
If your child has trouble breathing, swelling of the lips or tongue, or passes out - that’s anaphylaxis. Call 911 immediately. Antihistamines won’t stop this. Only epinephrine (EpiPen) can. Keep one on hand if your child has a known severe allergy.
But if your child has taken too much antihistamine - even if they seem sleepy - call Poison Control at 1-800-222-1222. Signs of overdose include:
- Extreme drowsiness or inability to wake up
- Racing heart or irregular heartbeat
- Very dry mouth or flushed skin
- Confusion, hallucinations, or agitation
- Difficulty urinating
Don’t wait. Don’t try to make them vomit. Just call. Poison control will guide you step by step.

What’s Changing in 2025?
Research is moving fast. In 2020, we didn’t have solid data for babies under 6 months. Now, doctors are starting to use cetirizine off-label in those infants - at 0.125 mg/kg - with good results. A large clinical trial (NCT04567821) is ongoing and could lead to FDA approval for babies as young as 3 months by 2026.
Meanwhile, pediatric hospitals across the U.S. are updating their protocols. Boston Children’s, St. Louis Children’s, and Children’s Hospital Colorado now all list cetirizine as first-line treatment for infants and toddlers with allergic reactions. Diphenhydramine is reserved for emergencies - like a sudden hive outbreak - and only when a doctor is involved.
Still, 28.7% of pediatric antihistamine use is off-label - mostly for kids under 2. And 62% of those cases involve Benadryl. That’s a problem. The data is clear: second-generation antihistamines are safer, more effective, and better tolerated. We need to stop treating kids like adults.
Final Checklist for Parents
Before giving any antihistamine to your child, ask yourself:
- Is this medicine approved for my child’s age? (Check the label.)
- Do I know my child’s exact weight? (Don’t guess - use a scale.)
- Am I using the measuring tool that came with the medicine?
- Is this a single-ingredient product? (Avoid cold + allergy combos.)
- Am I giving this for allergies - not for sleep?
- Have I checked the dose against a trusted source like Boston Children’s or AAAAI?
If you’re unsure, call your pediatrician or pharmacist. Don’t rely on internet advice. Every child is different. What worked for your neighbor’s kid might be too much for yours.
Can I give my 4-month-old Benadryl for hives?
No. The FDA warns against using diphenhydramine (Benadryl) in children under 2 years without a doctor’s order. For infants under 6 months, even cetirizine (Zyrtec) is used off-label and only under medical supervision. If your baby has hives, contact your pediatrician immediately. They may recommend a low dose of cetirizine or suggest other treatments. Never give Benadryl to a baby under 2 without professional guidance.
Is Zyrtec safer than Claritin for toddlers?
Both are safe for toddlers, but Zyrtec (cetirizine) works slightly faster and stronger for hives and allergic swelling. Claritin (loratadine) causes less drowsiness - about 7% of kids feel sleepy, compared to 15% with Zyrtec. If your child is prone to tiredness or has trouble sleeping, Claritin might be better. For active kids with severe allergies, Zyrtec is often preferred. Either is far safer than Benadryl.
How do I know if I’m giving the right dose?
Always base the dose on your child’s weight, not age. Use the measuring device that came with the medicine - never a kitchen spoon. Check the label for mg per mL (e.g., 5 mg/5 mL). Multiply your child’s weight in kg by the recommended dose per kg (e.g., 0.25 mg/kg for infants 6-11 months). If you’re unsure, ask your pharmacist to calculate it for you. Most pharmacies offer free dose checks.
Can I give antihistamines every day?
Yes - if it’s a second-generation antihistamine like cetirizine or loratadine, and it’s for chronic allergies like seasonal rhinitis or eczema. These are safe for daily use in children over 6 months (Zyrtec) or 2 years (Claritin). But never use them daily for colds or as sleep aids. Daily use should be under a doctor’s supervision, especially in children under 2.
What if my child accidentally takes too much?
Call Poison Control immediately at 1-800-222-1222. Do not wait for symptoms. Signs of overdose include extreme drowsiness, fast heartbeat, dry mouth, trouble urinating, confusion, or agitation. Keep the medicine bottle handy when you call - they’ll need to know the exact drug and amount taken. If your child is unconscious or having trouble breathing, call 911.
What Comes Next?
If your child has ongoing allergies, consider seeing a pediatric allergist. They can test for specific triggers - like dust mites, pet dander, or certain foods - and help you create a long-term plan. Antihistamines are a tool, not a cure. The goal is to reduce exposure, manage symptoms safely, and avoid unnecessary meds.
Keep a written record of what you give, when, and why. Note any side effects. That helps your doctor make better choices. And if you ever feel unsure - don’t guess. Call someone who knows. Your child’s safety is worth the extra step.


Just read this and I’m so glad I didn’t rely on internet advice when my daughter broke out in hives 🙌 I called the pediatrician immediately-no Benadryl, no guessing. We started her on 2.5mg cetirizine and it was like magic. Also, bought the dosing syringe from the pharmacy-$2 well spent. Don’t use kitchen spoons. Seriously. 🚫🥄
THIS. Is. CRITICAL. I used to think Benadryl was the go-to for everything-sleep, allergies, even car rides. Then my 3-year-old got so groggy he couldn’t walk straight after a dose. We switched to Zyrtec and he’s been running around like a maniac again. No more ‘baby sleeping pills’. Kids aren’t tiny adults. Stop treating them like they are.
As a mom of two kids with severe eczema and food allergies, I’ve seen the chaos of wrong dosing. One time, my son got a rash from a neighbor’s dog-my sister gave him Benadryl ‘because it worked for her kid’. He got so hyper and then crashed. We ended up in urgent care. Second-gen antihistamines are the future. We need to stop normalizing old-school habits. This post? A lifeline.
Always use the measuring tool. Always check weight. Always avoid combination products. These three rules saved my son’s health. I keep a printed dosing chart taped to the medicine cabinet. Simple. Clear. No guesswork. If you’re unsure, call your pharmacist. They’re trained for this. You don’t need to be.
ok so i just found out my 4 year old has been getting 10mg of zyrtec every day because i thought the kids tablet was the same as the adult one… and i’ve been doing this for 8 months… i feel like a terrible parent… i’m going to the pharmacy right now to get a new bottle and a syringe… thank you for this post… i didn’t know…
From the UK, I’ve seen similar trends here-parents reach for Benadryl because it’s cheap and familiar. But our NHS guidelines mirror the US: second-gen first. I shared this with my sister-in-law who’s just had her first baby. She’s now got the dosing chart on her fridge. Small actions, big impact.
Let’s be real-most parents aren’t medical professionals. We’re tired, overwhelmed, and trying to do the best we can with what we’ve got. But this isn’t about blame. It’s about access. Why is it so hard to get accurate dosing tools? Why do pharmacies charge $5 for a syringe? Why aren’t these included in every OTC allergy package by law? Why do we still have pediatric formulations with misleading labels? This post is a wake-up call, but systemic change is what we need. We need standardized dosing labels, free measuring tools with every bottle, and mandatory pharmacist counseling for parents buying antihistamines for kids under 6. Until then, we’re all just playing Russian roulette with our children’s health.
There is an epistemological tension here: the authority of clinical guidelines versus the lived experience of parental intuition. The data is clear-second-generation antihistamines reduce CNS penetration, minimize sedation, and align with pediatric pharmacokinetics. Yet cultural inertia persists, rooted in generational narratives of ‘Benadryl works for everything.’ This is not merely a medical issue-it is a semiotic one. The symbol of Benadryl as a panacea must be deconstructed through education, not just prescription. We must shift from pharmacological convenience to pharmacological responsibility.