
Diabetic retinopathy isn't just a complication of diabetes-it's the leading cause of preventable vision loss in working-age adults. If you have diabetes, your eyes are at risk. But here’s the good news: diabetic retinopathy can be caught early, and in most cases, vision loss can be avoided entirely. The key? Knowing when to get screened and what treatments actually work.
When Should You Get Screened for Diabetic Retinopathy?
Screening isn’t one-size-fits-all. The old rule of ‘get checked every year’ doesn’t apply to everyone anymore. New guidelines, backed by decades of research, now recommend personalized screening based on your risk level.
If you have type 1 diabetes, your first eye exam should happen 3 to 5 years after diagnosis. For type 2 diabetes, it’s recommended right after diagnosis because many people already have some level of retinal damage by the time they’re diagnosed with diabetes.
After your first exam, your doctor will decide your next steps based on what they find:
- No diabetic retinopathy: If your retina looks completely healthy and your blood sugar (HbA1c) is under control (below 7%), you can wait 1 to 2 years before your next exam. Some low-risk patients, especially those with type 2 diabetes and no other complications, may safely go up to 3 or even 4 years between screenings.
- Mild nonproliferative diabetic retinopathy (NPDR): This is the earliest stage. You’ll need to come back in 6 to 12 months. Tight control of blood sugar and blood pressure is critical here.
- Moderate NPDR: This means changes are becoming more noticeable. You’ll need to see an eye specialist every 3 to 6 months.
- Severe NPDR: This is a warning sign. You need to be evaluated by a retina specialist within 3 months.
- Proliferative diabetic retinopathy (PDR): New, fragile blood vessels are growing. This is serious. You need to see a specialist within 1 month.
There’s also a tool called RetinaRisk that uses your age, how long you’ve had diabetes, your HbA1c, blood pressure, and kidney function to calculate your personal risk. It can suggest screening intervals ranging from 6 months to 5 years. This isn’t just theory-studies show it reduces unnecessary screenings by nearly 60% without missing cases that need treatment.
Why Not Just Get Screened Every Year?
Annual screening sounds safe, but it’s not always necessary-and it’s not always practical. For people with stable diabetes and no signs of eye damage, yearly visits mean more time off work, more travel, more costs, and more stress.
A 2022 review of over 20,000 patients found that extending screening to every 2 or 3 years for low-risk individuals didn’t increase the chance of vision loss. In fact, the UK’s national screening program switched to biennial screening for low-risk patients and saw no rise in blindness cases.
But here’s the catch: if your HbA1c is above 8.5%, your blood pressure is over 140/90, or you have kidney disease, annual screening is still the standard. Risk stratification only works if your doctor knows your full health picture. Too many patients get pushed into longer intervals despite having uncontrolled diabetes-and that’s when things go wrong.
One Reddit user shared how their clinic extended their screening to every two years despite an HbA1c of 8.5%. Within a year, they developed diabetic macular edema. It could’ve been caught earlier.
What Happens During a Diabetic Retinopathy Screening?
A screening isn’t just a quick glance. It’s a detailed imaging process. Most clinics now use digital fundus photography-no poking, no discomfort. Your pupils are dilated with drops, and a special camera takes high-resolution photos of the back of your eyes. At least two images per eye are taken, covering the central and peripheral retina.
These images are graded using the International Clinical Diabetic Retinopathy Disease Severity Scale, which has five levels: no retinopathy, mild NPDR, moderate NPDR, severe NPDR, and proliferative DR. Diabetic macular edema (DME)-swelling in the central part of the retina-is assessed separately.
AI is now being used to analyze these images. Tools like Google’s DeepMind algorithm and IDx-DR can detect sight-threatening retinopathy with over 94% accuracy. Some clinics even use smartphone attachments like the D-Eye device, allowing primary care doctors to take retinal photos during a regular visit.
Telemedicine programs have made screening more accessible, especially in rural areas where eye specialists are scarce. One large study found tele-screening caught 94% of cases that needed referral-almost as good as an in-person exam.

Treatment Options for Diabetic Retinopathy
Not every case needs treatment. Mild retinopathy often just needs better control of blood sugar, blood pressure, and cholesterol. But when it progresses, there are three main treatments:
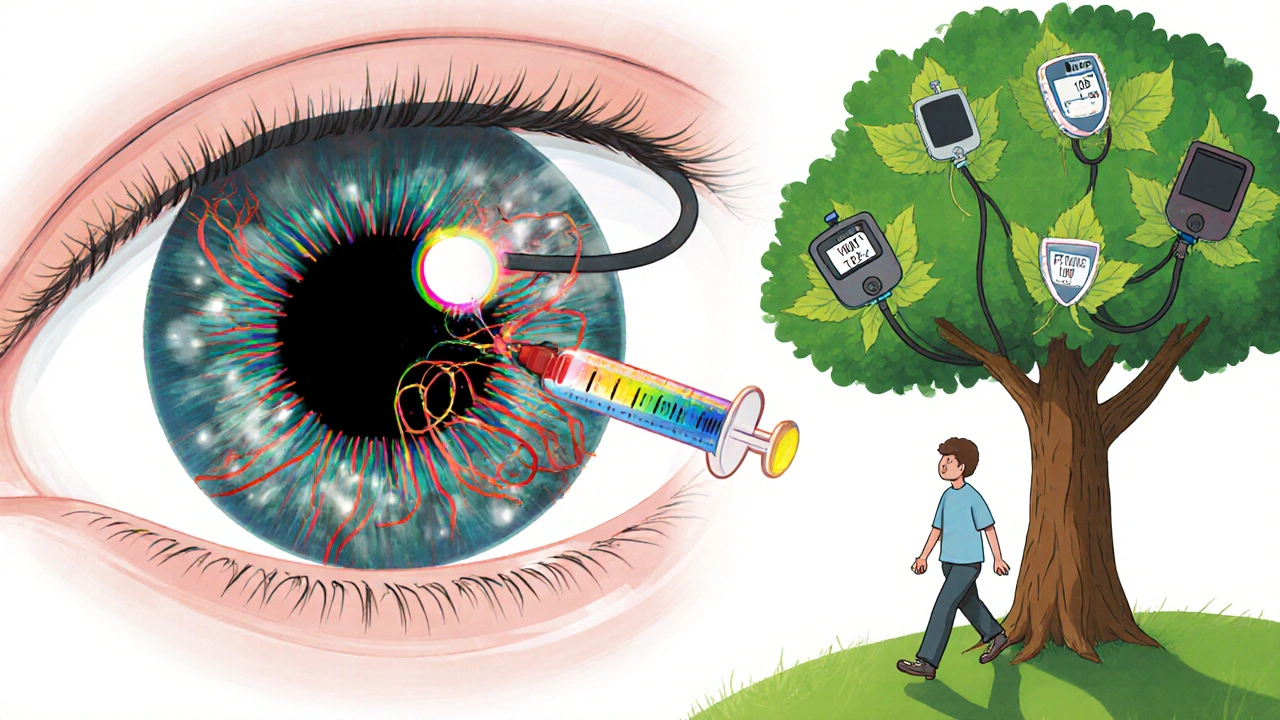
- Anti-VEGF injections: These are the most common treatment for diabetic macular edema and advanced retinopathy. Drugs like ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) are injected into the eye to stop abnormal blood vessels from leaking and growing. Most patients need 3 to 6 injections in the first year, then fewer over time. Studies show these injections can improve vision in 40-50% of patients with DME.
- Laser therapy: Focal laser treatment seals off leaking blood vessels in the macula. Panretinal photocoagulation (PRP) is used for proliferative retinopathy to shrink abnormal vessels. It’s less common now because anti-VEGF injections are more effective for vision improvement, but PRP still prevents severe vision loss in over 90% of cases.
- Vitrectomy: This is surgery to remove blood or scar tissue from inside the eye. It’s reserved for advanced cases with heavy bleeding or retinal detachment. Recovery takes weeks, and vision improvement isn’t guaranteed-but it’s often the last chance to save sight.
Early treatment is everything. The Early Treatment Diabetic Retinopathy Study showed that timely laser therapy reduced the risk of severe vision loss by 50%. Today, with anti-VEGF drugs, that number is even higher.
What You Can Do to Protect Your Vision
Screening and treatment are important-but they’re not your only defense. Your daily choices matter just as much:
- Keep your HbA1c under 7%. The DCCT study showed that intensive control reduced retinopathy risk by 76% in type 1 diabetes.
- Control your blood pressure. Aim for below 140/90. High blood pressure speeds up damage to the tiny blood vessels in your eyes.
- Manage your cholesterol. High triglycerides and LDL are linked to faster progression of retinopathy.
- Don’t smoke. Smoking doubles your risk of developing diabetic eye disease.
- Get regular exercise. Even 30 minutes of walking five days a week improves blood sugar control and circulation.
- Check your kidneys. Protein in your urine (microalbuminuria) is a red flag for retinopathy progression.
One patient in San Diego, diagnosed with type 2 diabetes in 2018, kept her HbA1c under 6.5% through diet, walking, and medication. Her retinopathy screenings have been clear every two years since 2020. She didn’t need a single injection. Her story isn’t rare-it’s the result of consistent care.
What’s Changing in Diabetic Eye Care?
The field is moving fast. AI screening tools are now FDA-cleared and being used in clinics across the U.S. The American Diabetes Association updated its 2024 guidelines to emphasize personalized screening, not fixed schedules. New point-of-care devices are making it easier for primary care offices to do basic screenings without sending patients to specialists.
Global efforts are scaling up too. The World Health Organization estimates that if risk-based screening is adopted worldwide, we could prevent 2.5 million cases of blindness from diabetes by 2030.
But disparities remain. Low-income communities and rural areas still have much lower screening rates. In the U.S., only 58-65% of people with diabetes get the recommended eye exams. Insurance coverage, transportation, and lack of awareness are big barriers.
Frequently Asked Questions
Can diabetic retinopathy be reversed?
Early damage from diabetic retinopathy can sometimes improve with treatment-especially if caught before the retina is permanently scarred. Anti-VEGF injections and laser therapy can reduce swelling and stop bleeding, leading to vision improvement in many cases. But once the retina has developed significant scarring or nerve damage, vision loss is usually permanent. That’s why early detection is so critical.
Do I need to see an eye doctor if I have no symptoms?
Yes. Diabetic retinopathy often has no symptoms in the early stages. By the time you notice blurry vision, floaters, or dark spots, the disease may already be advanced. That’s why regular screenings-even if you feel fine-are the only way to catch it early.
How often should I get screened if I have type 1 diabetes?
Start screening 3 to 5 years after diagnosis. If your retina is healthy and your HbA1c is under 7%, you can extend screening to every 1 to 2 years. If you have any signs of retinopathy, you’ll need more frequent follow-ups. The American Diabetes Association now supports risk-based scheduling, not just annual exams.
Is diabetic retinopathy screening covered by insurance?
Yes, in most cases. Medicare covers annual diabetic eye exams for people with diabetes. Most private insurers also cover screening under preventive care benefits. If you’re on Medicaid or have a high-deductible plan, check with your provider-but many clinics offer sliding-scale fees or free screenings through public health programs.
Can pregnancy affect diabetic retinopathy?
Yes. Pregnancy can speed up the progression of diabetic retinopathy, especially if blood sugar isn’t tightly controlled. Women with diabetes who are pregnant or planning to become pregnant should have an eye exam in the first trimester and may need follow-ups every 3 months during pregnancy. Postpartum screening is also recommended, as changes can continue for months after delivery.
Are there any new treatments on the horizon?
Yes. Researchers are testing longer-lasting anti-VEGF drugs that require fewer injections. There’s also early work on implantable devices that slowly release medication into the eye. Gene therapy and stem cell treatments are still experimental, but they offer hope for future options. The biggest advance right now is better screening-catching problems before they need complex treatment.
Next Steps: What to Do Now
If you have diabetes and haven’t had an eye exam in the last year, schedule one now. Don’t wait for symptoms. Bring your latest HbA1c results, blood pressure readings, and kidney function tests-these help your doctor decide your screening interval.
If you’ve been told you can wait two years for your next exam, ask: ‘What’s my risk level? What factors could change that?’ Make sure your doctor is using current guidelines, not outdated annual schedules.
And if you’ve been diagnosed with retinopathy, don’t panic. With the right treatment and lifestyle changes, most people keep their vision. Stay consistent. Keep your numbers in range. Show up for your appointments. Your eyes are worth it.


Man, this post is a godsend. I’ve been dodging eye checks for years thinking ‘I feel fine’ - turns out my HbA1c was flirting with 8.2 and my retina was throwing silent tantrums. Got screened last month - mild NPDR. Now I’m walking 10k steps daily, ditching soda, and actually reading my lab reports. Who knew diabetes wasn’t just about insulin and bagels?
Of course the government and big pharma want you to get screened every year - more tests, more $$$ for the system. Real solution? Cut sugar. Stop taking pills. Go keto. I’ve seen 3 people reverse their diabetes in 6 months. Why are we letting corporations profit off your blindness?
As someone raised in a household where preventive care was non-negotiable, I’m deeply moved by the precision of these guidelines. The integration of RetinaRisk and AI diagnostics reflects a global shift toward data-driven, patient-centered medicine - not just in the U.S., but in places like India and Kenya, where teleophthalmology is bridging gaps in access. This isn’t just medicine; it’s equity in action.
Important note: if your clinic is pushing you to 2-year intervals and your HbA1c is above 7.5% - push back. Seriously. I had a friend who got the ‘low-risk’ label despite uncontrolled glucose - she developed DME in 8 months. Don’t let a spreadsheet override your body’s warning signs. Ask for your risk score. Demand transparency.
So let me get this straight - you’re telling me I can skip my eye exam for 3 years if I’m ‘low risk’? 😳 Meanwhile, my cousin lost 70% of his vision because his doctor trusted a computer algorithm. Who’s to blame? The AI? The doctor? The system? I’m just glad I’m not the only one who thinks this is a gamble with eyeballs.
My dad’s had type 2 since 2005. Never had an issue. Got his first screening last year - zero retinopathy. HbA1c 6.1. Walks 5 miles every morning. No meds. Just food, discipline, and a stubborn refusal to be a statistic. Proof that it’s not about luck - it’s about showing up.
Let’s be clear: the ADA’s new guidelines are a cost-cutting measure disguised as personalized medicine. They’re not saving you money - they’re saving insurance companies money. And when someone loses vision because they were told ‘you’re low-risk,’ who takes responsibility? The algorithm? The doctor? Or the system that prioritized profit over prevention?
Anti-VEGF injections cost $2000 a pop and you need 6 of them in the first year. Meanwhile my cousin got a free screening at a Walmart clinic and they caught his PDR early. Why are we paying for luxury treatments when prevention is free? Stop spending money on fixing problems you could’ve stopped with a walk and a salad
AI screening? Big Tech is watching your retinas now. Google’s DeepMind? That’s the same company that sold health data to insurers. Next thing you know, your insurance premium goes up because your retina shows ‘early signs of neglect.’ This isn’t medicine - it’s surveillance with a stethoscope
It’s funny how we treat diabetes like a moral failure - ‘if you just ate better, you wouldn’t have this.’ But we don’t say that to people with heart disease or cancer. Why is the eye the last frontier of blame? Maybe the real disease isn’t in the retina - it’s in the way we judge people for being sick.
My uncle in Delhi got screened via smartphone camera at a local pharmacy - ₹200, no waiting, no specialist. AI flagged his PDR. He got treated in time. Tech isn’t the enemy. Access is. We need this everywhere - not just in Silicon Valley. 🌍👁️
The paradigm shift from time-based to risk-stratified screening represents a non-linear evolution in ophthalmic epidemiology - leveraging multivariate logistic regression models anchored in longitudinal biomarkers (HbA1c, eGFR, BP) to optimize resource allocation while preserving visual acuity endpoints. The reduction in unnecessary referrals is not merely statistical - it’s a systemic reconfiguration of preventive care economics.