
Medication Guide Distribution Checker
Check Distribution Requirements
Determine if a Medication Guide is required based on your setting and patient scenario
When you pick up a prescription for a high-risk medication, you might be handed a small paper booklet with bold warnings and simple instructions. That’s a Medication Guide-and it’s not optional. For certain drugs, the FDA requires it to be given to every patient, every time, under specific rules. But here’s the catch: not every pharmacy, clinic, or provider follows the same steps. Confusion is common. And when rules are unclear, patients miss critical safety info.
What Exactly Is a Medication Guide?
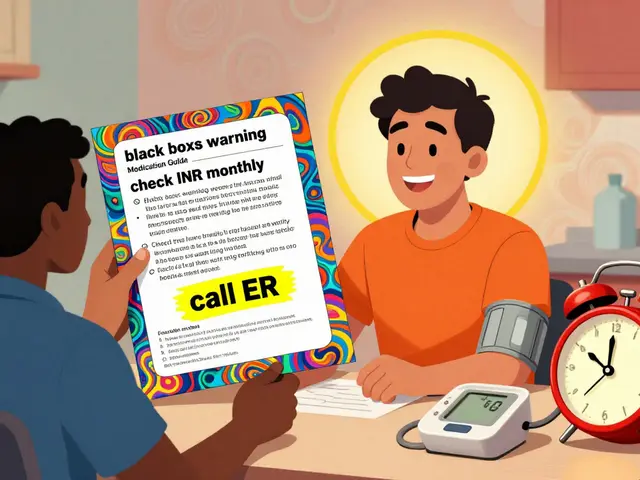
A Medication Guide (MG) is a printed handout approved by the FDA for specific prescription drugs with serious risks. Unlike general patient info sheets you might find online, these are legally required, drug-specific, and written in plain language. They’re not suggestions. They’re part of the drug’s official labeling. The FDA only requires a Medication Guide if the drug meets one of three criteria: it could cause serious harm if not used correctly, the risks outweigh the benefits in ways patients need to understand, or patient adherence is vital for the drug to work. Think drugs like isotretinoin (Accutane) for acne, clozapine (Clozaril) for schizophrenia, or estrogen-based therapies. Over 200 drugs currently need them. These guides explain side effects, what to avoid, signs of danger, and when to call a doctor. They’re designed so someone without a medical degree can understand them. But if they’re not handed out properly, they’re useless.When Must Pharmacists Give Out a Medication Guide?
Pharmacists are on the front lines. But they don’t have to hand out a guide every single time a patient gets the same prescription. The rules depend on the setting and the drug’s status. In a community pharmacy, if the patient is taking the drug at home-for example, a monthly injectable for multiple sclerosis-the Medication Guide must be given each time the prescription is filled. No exceptions. But in outpatient clinics, like an infusion center or dialysis unit, the rule changes. You only give the guide the first time the patient receives the drug. After that, unless the guide itself has been updated, you don’t need to hand it out again. This avoids cluttering patients with the same paper every week. There are five specific triggers that require distribution:- The patient or their agent asks for it.
- The drug is dispensed for self-administration in an outpatient setting (like at home).
- This is the first time the drug is given to a patient in a clinic or infusion center.
- The Medication Guide has been revised by the FDA and new content is added.
- The drug is part of a REMS program (Risk Evaluation and Mitigation Strategy) that specifically requires it.
What About Hospitals and Nursing Homes?
Here’s a common misunderstanding: Medication Guides are NOT required in inpatient settings. If a patient is admitted to a hospital or lives in a nursing home, pharmacists don’t need to hand out printed guides during their stay. But that doesn’t mean no education happens. Providers still need to verbally explain risks, side effects, and what to watch for. The difference? The FDA doesn’t mandate a printed guide in those environments. The responsibility shifts from paper to conversation. This creates a gap. Patients discharged from the hospital might leave without ever seeing the guide, even if they’ll take the drug at home. That’s why some hospitals now print and give the guide at discharge as a best practice-even if it’s not legally required.
Medication Guides vs. Other Patient Info
Not all patient handouts are the same. You might see terms like Patient Medication Information (PMI) or Consumer Medication Information (CMI). These are often created by pharmacies or third parties. They’re helpful, but they’re not FDA-approved. They can be generic, outdated, or missing key warnings. Medication Guides are different. They’re developed by drug manufacturers under FDA oversight, reviewed for accuracy, and must include specific safety content. They’re the only patient-facing documents with federal backing. Also, don’t confuse them with package inserts. Those are for doctors-dense, technical, full of clinical data. Medication Guides are for patients. Short sentences. Clear headings. Bullet points. No jargon.Why Do These Rules Even Exist?
The goal is simple: prevent harm. Drugs like clozapine can cause a life-threatening drop in white blood cells. Isotretinoin can cause severe birth defects. If a patient doesn’t know the risks-or forgets them-they might skip blood tests or get pregnant without realizing the danger. Dr. Janet Woodcock, former head of the FDA’s drug center, called Medication Guides “essential tools that help patients understand serious risks.” Studies show patients who receive them are more likely to report side effects and follow safety steps. But here’s the problem: many patients don’t read them. A 2022 study found only 37% could recall key safety points a week after getting the guide. That’s not because the guides are bad-they’re well-written. It’s because they’re handed out in a rush, often ignored, or not discussed. That’s why some experts say the system needs work. Dr. Lucinda Maine, former ASHP executive, pointed out that the administrative burden doesn’t always match the safety payoff. But removing them? That’s not the answer.What Are Pharmacists Doing Right-and Wrong?
A 2022 survey of over 1,200 hospital pharmacists found 68% were confused about when to hand out guides in outpatient clinics. Nearly half admitted they sometimes gave them out unnecessarily just to be safe. On Reddit, pharmacists in infusion centers ask: “Do we give the guide for epoetin alfa every week or just once?” The answer? Once-unless the guide changed. But without clear protocols, many give it every time. The fix? Systems. The University of California San Francisco Medical Center cut distribution errors by 73% by linking their pharmacy software to a barcode scanner. When a drug requiring a guide is scanned, the system pops up a reminder: “Print Medication Guide.” No guesswork. No missed steps. Other clinics now train staff on the five triggers. They keep printed copies of current guides on hand. They update their policies every time the FDA releases a revised version.
What’s Changing in 2025?
The FDA is pushing for more electronic options. In May 2023, they proposed allowing patients to receive Medication Guides via email, app, or patient portal-so long as they can still get a paper copy if they ask. This makes sense. Younger patients prefer digital. But older adults, especially those on multiple medications, still rely on paper. So the rule remains: paper must be available. Electronic is an option, not a replacement. Also, the number of drugs needing guides is rising. Evaluate Pharma predicts a 22% increase over the next five years, mostly in cancer and rare disease drugs. More specialty meds = more complex risks = more need for clear patient info. The FDA is also reviewing whether the program works as intended. A congressionally mandated study is due by late 2024. It could lead to changes in which drugs require guides, how they’re formatted, or how they’re delivered.What You Should Do as a Provider or Pharmacist
If you’re dispensing a drug that requires a Medication Guide:- Know the five triggers. Write them down. Post them near the counter.
- Check the FDA’s current list of drugs with guides. It updates regularly.
- Track revisions. When the FDA approves a new version, update your stock immediately.
- Don’t assume patients read it. Briefly point out the most important warning: “This guide says you need weekly blood tests. Don’t skip them.”
- Use technology. If your pharmacy system can flag guide-required drugs, use it.
- For outpatient clinics: give the guide once. Unless it changed. Then give it again.
Final Thought
Medication Guides aren’t perfect. They’re not always read. They’re not always given correctly. But they’re one of the few federal tools designed to put life-saving info directly into patients’ hands. For pharmacists and providers, understanding the rules isn’t about compliance-it’s about preventing avoidable harm. Get it right, and you’re not just following the law. You’re changing outcomes.Do I have to give a Medication Guide every time a patient refills a prescription?
Only if the drug is for self-administration at home. In community pharmacies, yes-every refill requires a new printed guide. But in outpatient clinics like infusion centers, you only give it the first time the patient receives the drug, unless the FDA updates the guide.
Are Medication Guides required in hospitals?
No. The FDA does not require Medication Guides to be distributed in inpatient settings like hospitals or nursing homes. However, staff must still verbally educate patients on risks and proper use. Many hospitals choose to provide the guide at discharge as a best practice.
Can patients get Medication Guides electronically?
Yes, as of 2023, the FDA proposed allowing electronic delivery via email, patient portals, or apps-but only if patients can still request a paper copy. The paper version must always be available. Electronic delivery is an option, not a replacement.
How do I know if a drug requires a Medication Guide?
Check the FDA’s official list of drugs with approved Medication Guides. It’s updated regularly on the FDA’s website. Pharmacies should also maintain a current internal list and train staff on how to identify these drugs by name or NDC code.
What’s the difference between a Medication Guide and a package insert?
A Medication Guide is written in plain language for patients and approved by the FDA. A package insert is the technical, detailed document meant for healthcare professionals, with dosing, clinical trial data, and pharmacokinetics. They serve different audiences and purposes.
Do Medication Guides replace patient counseling?
No. They’re a supplement, not a substitute. Pharmacists and providers must still counsel patients on how to take the drug, what side effects to watch for, and when to seek help. The guide supports that conversation-it doesn’t replace it.


Just got prescribed methotrexate last week and no guide was given. Asked for it and the pharmacist looked at me like I asked for a unicorn. Said 'we don't usually hand those out unless it's something like Accutane.' Guess I'm lucky I know to ask.
As a pharmacist in Mumbai, I can confirm the confusion is real. We get the same guides from distributors but rarely have clear protocols. Some staff give them every refill, others only if asked. We just started tagging high-risk drugs in our system with a red flag and it cut errors by half. FDA should mandate digital alerts in pharmacy software globally.
Let’s be real - this entire system is a bureaucratic farce. You’re telling me a 72-year-old with dementia is going to read a 3-page guide printed in 8pt font while the pharmacist is yelling at the next customer? The real issue isn’t distribution - it’s that we outsource patient safety to paper while ignoring cognitive load, literacy gaps, and systemic understaffing. The FDA’s solution is to print more pamphlets instead of fixing the damn system. Pathetic.
My mom had clozapine and the guide saved her life. She didn’t understand why she needed weekly blood draws until she read the part about agranulocytosis. We kept it taped to the fridge. I wish every high-risk med came with one - even if people don’t read them, at least they’re there when they need them.
They want to give these guides electronically now? Next they’ll be forcing us to get our meds through Big Pharma apps that track our heartbeat and sell our data. This is how they control us. Paper is freedom. If I want to read a guide I’ll print it myself. No corporate tracking. No spy software. Stay off my meds, Silicon Valley.
Why do we even bother with these things? Half the patients throw them in the trash. The other half forget what they read. I’ve been a pharmacist for 15 years and I’ve never seen one actually change behavior. Just give the verbal warning and move on. This is just paperwork theater to make regulators feel good
Anyone who thinks Medication Guides are effective hasn’t worked in a rural pharmacy. People don’t read. They don’t understand. The guides are written for college grads but most patients are on Medicaid with a 6th grade reading level. The FDA doesn’t care. They just want to check a box. Real safety is face-to-face counseling - not a folded piece of paper.
Just got my first isotretinoin guide and I cried. Not because I was scared - because someone finally cared enough to write it in words I could understand. 🥹 Thank you to the pharmacists who still hand them out even when they’re rushed. You’re doing god’s work.
There’s a critical gap between the FDA’s requirements and real-world implementation. In hospitals, verbal counseling is legally sufficient, but it’s inconsistently documented. We’ve started using standardized scripts for high-risk meds and recording them in the EHR. Patients who received structured counseling had 40% fewer readmissions. Paper guides help, but human interaction is the real safety net.
Let’s cut the nonsense. The entire Medication Guide system is a relic of the 1990s. We live in 2025. No one reads paper handouts anymore. Young people use apps. Elderly people forget where they put things. The FDA’s insistence on paper is not patient-centered - it’s liability-driven. And don’t get me started on the fact that some guides are written by marketing teams with no clinical input. Half of them are vague, contradictory, or outdated by the time they’re printed. This isn’t safety - it’s performative compliance wrapped in glossy paper. If you want real change, make the guides interactive, audio-enabled, and tied to refill reminders. Or stop pretending this is helping anyone.
My clinic gives the guide once then files it. We don’t print every time because it wastes paper and confuses patients. The FDA doesn’t say you have to hand it out every time - just when the criteria are met. Stop overdoing it. You’re not helping. You’re just making more trash