Psoriasis Treatment: Options, Tips, and What Works
When dealing with Psoriasis Treatment, the set of medical and self‑care strategies aimed at reducing skin inflammation, scaling, and discomfort. Also known as psoriasis therapy, it helps people manage a chronic skin condition that affects millions worldwide. Accurate diagnosis of psoriasis, a lifelong immune‑driven disease, is the first step before any therapy can be chosen.
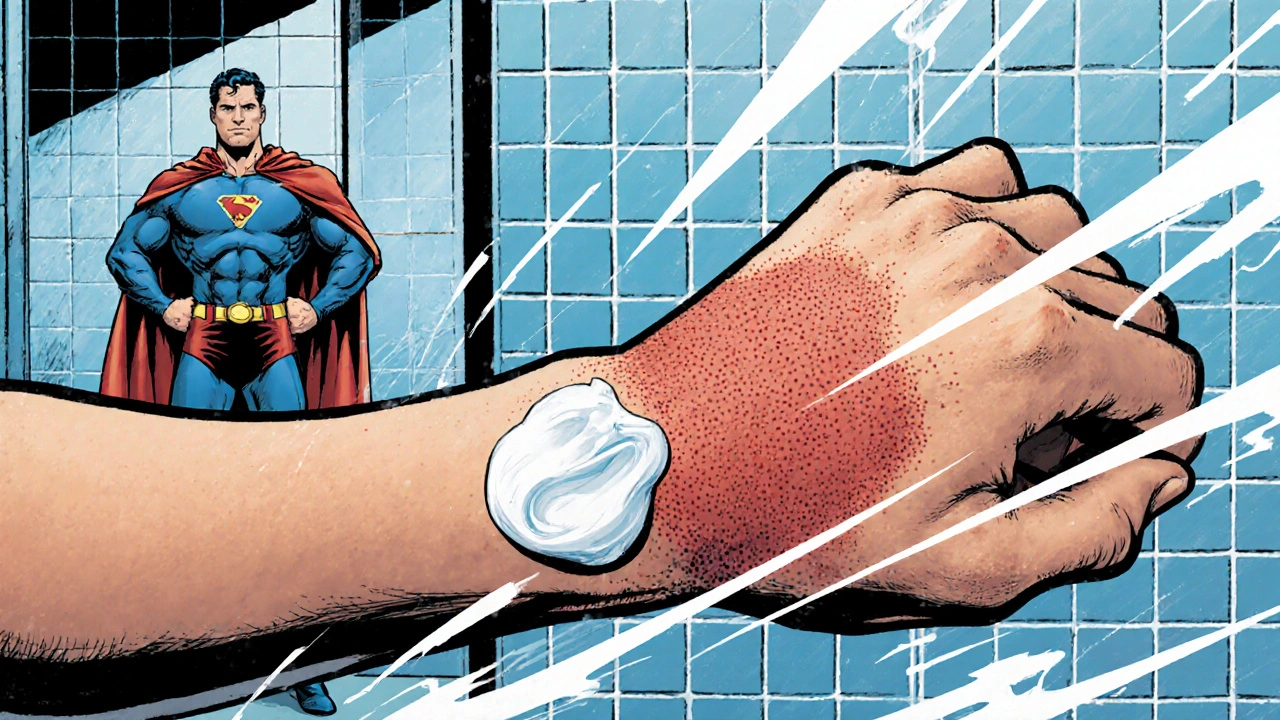
Psoriasis Treatment encompasses several distinct approaches. Topical therapy is the most common entry point; corticosteroid creams, vitamin D analogues, and retinoids work directly on the skin to calm flare‑ups. For moderate to severe cases, biologic drugs, such as adalimumab and ustekinumab, target specific immune pathways and have reshaped outcomes for many patients. Phototherapy, which uses controlled UV light, offers a middle ground—effective for many without the systemic exposure of biologics. Lifestyle management, including stress reduction, diet tweaks, and moisturising routines, supports any medical plan and can lower the frequency of relapses.
How These Options Interact
Psoriasis treatment requires a layered strategy: (1) accurate diagnosis informs which modality fits; (2) topical agents often serve as the first line, especially for mild patches; (3) phototherapy steps in when topical relief wanes; (4) biologic drugs are reserved for extensive disease or when other measures fail. This hierarchy mirrors the semantic triple "Psoriasis treatment includes topical therapy", "Phototherapy complements systemic options", and "Biologic drugs target immune pathways". Each option also influences the next—effective moisturising can improve topical absorption, while reduced inflammation from biologics can make phototherapy sessions shorter.
Choosing the right mix depends on age, disease extent, insurance coverage, and personal preferences. Young adults often start with over‑the‑counter creams but may transition to prescription steroids if plaques persist. Patients with joint involvement (psoriatic arthritis) might prioritize biologics early to protect both skin and joints. Seasonal changes also matter; many report flares in winter, prompting a shift toward richer moisturisers and occasional light therapy. Understanding these dynamics helps you weigh benefits against potential side effects, such as steroid thinning, UV‑related skin aging, or infection risk with immunosuppressive biologics.
Beyond medication, practical steps boost any treatment plan. Keep skin moisturised at least twice daily, avoid harsh soaps, and use lukewarm water to prevent barrier damage. Stress‑management techniques—mindfulness, regular exercise, or hobbies—can lower flare frequency because stress hormones fuel inflammation. When you start a new biologic, regular lab monitoring ensures safety and lets your doctor adjust dosing promptly. And always discuss travel plans with your clinician; phototherapy schedules may need tweaking, and biologic storage requirements differ from topical meds.
Below you’ll find a curated collection of articles that dive deeper into each of these areas. Whether you’re looking for a step‑by‑step guide on topical creams, the latest research on biologic agents, practical phototherapy tips, or lifestyle hacks to keep your skin calm, the posts ahead cover the full spectrum of psoriasis treatment strategies.
Learn how calcipotriene works, its common and rare side effects, safety tips, and when to combine it with steroids for best results.