Calcipotriene Risk Calculator
This calculator estimates your risk of hypercalcemia (elevated calcium levels) while using Calcipotriene cream. Based on your usage patterns and health factors, it helps you determine when to get blood tests for calcium levels.
Remember: Severe hypercalcemia is rare but can be dangerous. Blood tests are recommended after 4-6 weeks of continuous use, especially if you have kidney issues.
Results will appear here after you calculate risk
If you’ve been prescribed a cream for plaque psoriasis, you’ve probably heard the name Calcipotriene is a synthetic vitamin D3 analog that you apply to the skin to slow down the rapid growth of skin cells. While many patients see clear improvements, the drug isn’t without its quirks. Knowing what to expect, how to spot a problem early, and when to call your doctor can make the difference between smooth relief and an unwanted reaction.
Key Takeaways
- Calcipotriene works by mimicking vitamin D, which helps normalize skin cell turnover.
- Most users experience mild irritation; severe reactions are rare but can include hypercalcemia.
- Apply a thin layer once or twice daily, avoid broken skin, and keep the area covered with a bandage only if advised.
- Regular lab checks are recommended for long‑term users, especially if you have kidney issues.
- Combining Calcipotriene with a topical corticosteroid often improves results and reduces irritation.
What Is Calcipotriene?
Calcipotriene belongs to the class of vitamin D analogs used mainly for plaque psoriasis. It was first approved by the U.S. Food and Drug Administration (FDA) in 1997 after several clinical trials demonstrated its ability to reduce scaling and redness. The cream is sold under brand names like Dovonex, but the generic version is widely available at a lower cost.
How Calcipotriene Works
The drug binds to vitamin D receptors in skin cells, telling them to slow down proliferation and to mature properly. In plain terms, it nudges the skin’s growth cycle back to normal, which is why plaques become thinner and less inflamed. This mechanism is different from that of topical steroids, which mainly suppress inflammation. Because Calcipotriene targets cell growth, it can be used for longer periods without the skin‑thinning side effects seen with steroids.
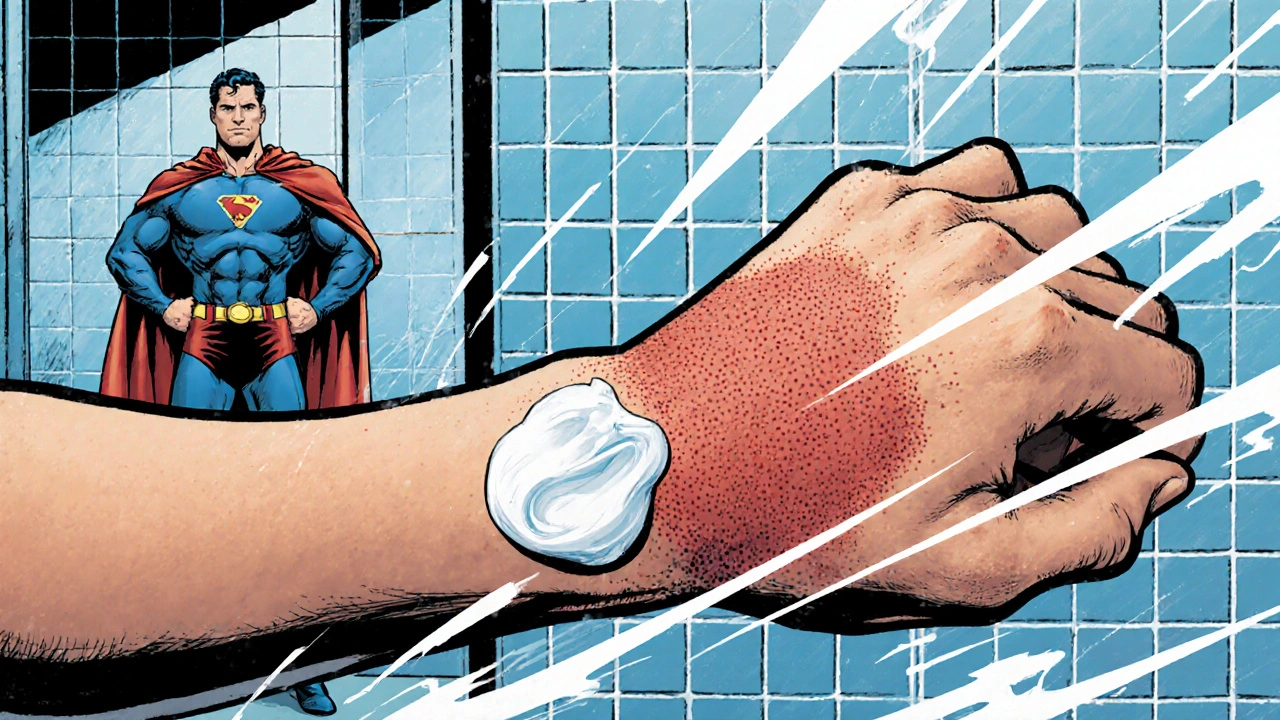
Common Side Effects
Most people notice only mild irritation. Typical complaints include:
- Redness at the application site
- Itching or burning sensation
- Dry, flaky skin
- Stinging when the cream contacts open cuts
These reactions usually fade within a week as your skin gets used to the medication. If they persist, trimming the dose to once a day or using a moisturizer underneath can help.
Rare but Serious Risks
While uncommon, some users experience more serious problems. Keep an eye out for the following warning signs:
- Hypercalcemia - elevated calcium levels in the blood. Symptoms can include nausea, increased thirst, frequent urination, and muscle weakness.
- Severe skin reactions such as erythema multiforme or allergic contact dermatitis
- Unexplained joint pain, which could signal systemic absorption
Because Calcipotriene is a vitamin D analog, it can raise calcium if you use large amounts or apply it to large body surfaces. Doctors usually order a blood calcium test after 4-6 weeks of continuous use, especially for patients with kidney disease.
Safety Tips & Monitoring
- Start with a thin layer on a small patch of skin. Wait 48 hours to see how you react before treating larger areas.
- Never apply the cream to broken skin, mucous membranes, or the face unless your doctor says it’s okay.
- Wash your hands thoroughly after each application to avoid accidental eye or mouth exposure.
- Keep the product out of reach of children - ingestion can cause dangerous spikes in calcium.
- Schedule blood work after the first month and then every 3-6 months if you stay on therapy.
- If you’re pregnant or nursing, discuss alternatives; animal studies suggest potential risks, although human data are limited.
Following these steps dramatically lowers the chance of hitting a serious issue.
Drug Interactions & Precautions
Calcipotriene doesn’t interact with most oral medications, but it can add up with other sources of vitamin D or calcium. Tell your doctor if you’re taking:
- Calcium supplements or multivitamins with high vitamin D content
- Thiazide diuretics, which can also raise calcium levels
- Other topical treatments that contain steroids, especially if you’re using them on the same spot
Patients with a history of kidney stones, sarcoidosis, or granulomatous diseases should be extra cautious, as these conditions already predispose them to high calcium.
Combination Therapy: Calcipotriene + Topical Steroid
Many dermatologists pair Calcipotriene with a low‑potency topical corticosteroid (often betamethasone). The steroid counters irritation, while Calcipotriene does the heavy lifting on cell growth. Below is a quick snapshot of how the two approaches compare.
| Feature | Calcipotriene Only | Calcipotriene+Betamethasone |
|---|---|---|
| Typical Strength | 0.005% cream | 0.005% Calcipotriene / 0.064% Betamethasone |
| Application Frequency | Once or twice daily | Once daily (combined) |
| Primary Benefit | Reduces plaque thickness | Reduces plaque thickness+less irritation |
| Common Mild Side Effects | Redness, itching | Redness, itching (often milder) |
| Rare Serious Risks | Hypercalcemia | Hypercalcemia (similar risk) + steroid‑related skin thinning if used >4weeks |
| Monitoring Needed | Blood calcium after 4‑6weeks | Blood calcium + skin check for steroid effects |
Most patients start with Calcipotriene alone. If irritation becomes a barrier, the doctor may add the steroid for a short 2‑week boost, then taper back to the vitamin D analog alone.
Frequently Asked Questions
Can I use Calcipotriene on my face?
Only if a dermatologist says it’s safe. The facial skin is thinner, so irritation and systemic absorption are higher. Most doctors prefer a lower‑strength formulation or a short trial period.
How long does it take to see results?
Visible improvement often appears within 2‑4weeks, but the full effect can take up to 12weeks of consistent use.
Do I need blood tests while using this cream?
Yes, especially the first few months. A baseline calcium level and a follow‑up after 4-6weeks help catch early hypercalcemia.
Can I combine Calcipotriene with other psoriasis meds?
It’s generally safe to use alongside systemic agents like methotrexate, but you should coordinate with your doctor to monitor overall vitamin D levels.
What should I do if I develop severe burning or swelling?
Stop using the cream immediately and contact your dermatologist. Severe local reactions may require a short course of oral steroids or a switch to an alternative therapy.
Is Calcipotriene safe for children?
It’s FDA‑approved for ages 12 and up. Younger children may need lower doses and closer monitoring.
Understanding calcipotriene side effects isn’t about scaring yourself; it’s about staying ahead of problems so you can keep enjoying clearer skin. If you follow the dosing tips, watch for red flags, and keep regular check‑ups, Calcipotriene can be a safe and effective part of your psoriasis toolkit.
Releted Post
15 Oct 2025

Calcipotriene indeed offers a valuable option for many battling plaque psoriasis, especially when paired with a low‑potency steroid to mitigate irritation 😊. The guide rightly stresses the importance of monitoring calcium levels, which can be overlooked in routine practice. Applying a thin layer to intact skin and washing hands afterward are simple yet crucial steps. Overall, a well‑balanced summary for patients and clinicians alike.
You really should read the safety section before slapping any cream on your skin. Ignoring the blood‑test recommendations is just reckless.
When it comes to Calcipotriene, the first thing to understand is that the molecule mimics the active form of vitamin D, binding to nuclear receptors on keratinocytes and thereby normalizing the proliferative cycle of the epidermis. This mechanism is fundamentally different from that of corticosteroids, which primarily suppress inflammation without addressing the underlying hyperproliferation. Because of this, patients can often remain on Calcipotriene for extended periods without the skin‑thinning side effects that limit steroid use. Nevertheless, the therapeutic benefit is closely tied to adherence to proper application technique, which includes using a pea‑sized amount for a localized plaque and avoiding broken skin or mucous membranes. Failure to respect these boundaries can increase systemic absorption, raising serum calcium and potentially precipitating hypercalcemia. Routine monitoring of serum calcium and renal function is therefore not a mere recommendation but a clinical necessity for anyone on long‑term therapy. In practice, I schedule baseline labs before initiation, followed by repeat testing at six weeks and then every three to six months, adjusting the interval based on the patient’s renal status and dosage. Should the calcium rise above the upper limit of normal, the immediate step is to reduce the frequency of application or pause therapy entirely, rather than pushing through discomfort. Concurrent vitamin D supplementation should also be curtailed, because the additive effect can tip the balance toward toxicity. If a patient experiences persistent erythema or burning, a short course of a low‑potency topical steroid can be added to the regimen, but this adjunct should be limited to two weeks to avoid steroid‑induced atrophy. Dermatologists often employ a “step‑down” approach, beginning with combination therapy to achieve rapid control, then tapering back to Calcipotrione monotherapy once the plaques have softened. Educating patients on the signs of hypercalcemia-such as polyuria, fatigue, and muscle weakness-empowers them to seek timely medical attention. It is equally important to advise them on lifestyle measures that can blunt calcium spikes, like limiting high‑calcium foods and avoiding excessive sunlight exposure that can boost endogenous vitamin D synthesis. Ultimately, the safety profile of Calcipotriene is favorable when these precautions are observed, and the drug remains a cornerstone in the armamentarium against plaque psoriasis. Failure to follow these guidelines, however, converts a benign topical agent into a potential systemic hazard. Therefore, a disciplined, protocol‑driven approach is essential for maximizing benefit while minimizing risk.
Excellent summary! The emphasis on regular calcium monitoring is spot‑on, and I appreciate the clear dosing instructions. Just a quick note: “the cream is sold under brand names like Dovonex” should be preceded by “The cream”. Keep up the great work!
Regarding the “simple steps” you mentioned, let’s unpack the pharmacokinetic variables: percutaneous absorption rates, stratum corneum integrity, and local vasoconstriction all modulate systemic bioavailability. Overlooking these parameters could skew the risk–benefit calculus.
Wow, that was a deep dive! 😊 I totally agree that those factors matter, especially when we’re trying to keep the dosing safe and effective. Thanks for breaking it down in a friendly way!
One could argue that the moral imperative to read safety data stems from our collective responsibility to preserve bodily integrity; neglecting such guidance is a subtle rebellion against the very notion of self‑care, a tragedy of modern complacency.
i think ur point is totally right but sometimes ppl just skip the labs cuz they r busy or dont get the reminder lol
Indeed, the ethical dimension you invoke resonates with the ancient Hippocratic ideal that “first, do no harm”-a principle that, when applied to topical therapeutics, mandates vigilant monitoring and informed consent; otherwise, we risk drifting into a nihilistic disregard for patient autonomy.
Great info-thanks for the clear rundown!