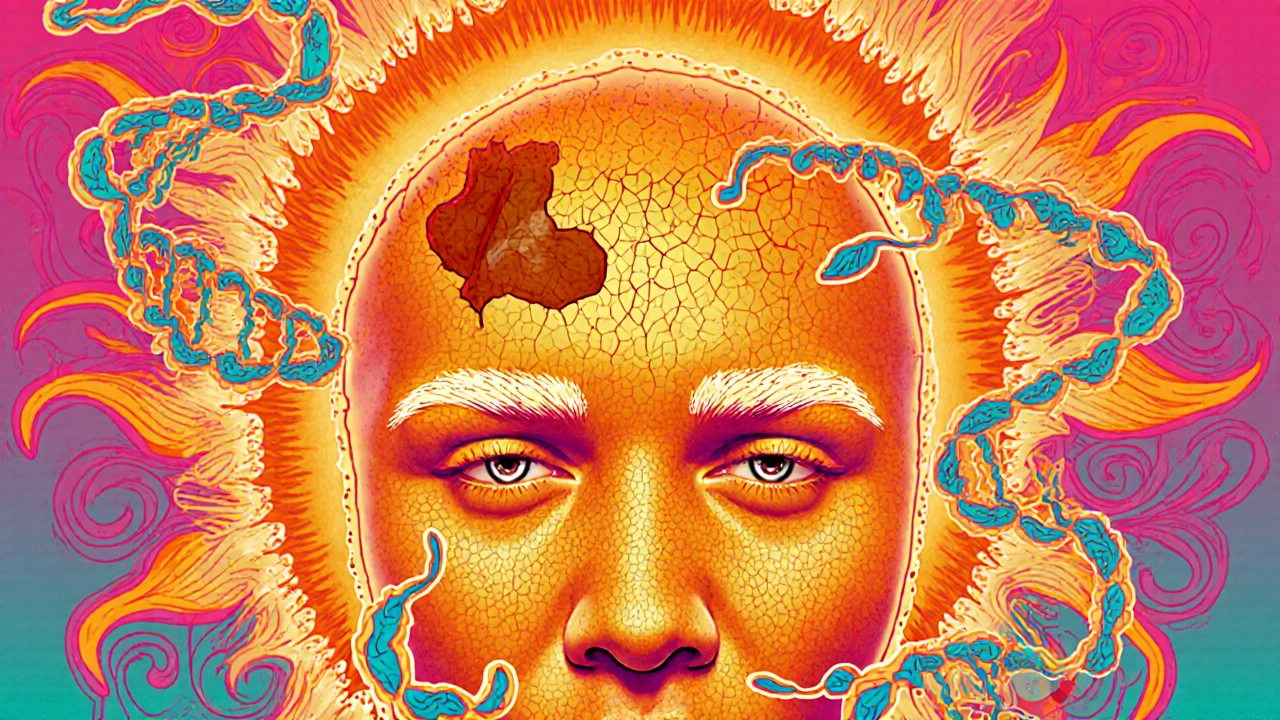
Most people don’t realize that a rough, dry patch on their cheek or scalp could be more than just sun-damaged skin. It could be an actinic keratosis - a precancerous lesion that, if ignored, might turn into skin cancer. These aren’t rare. In the U.S. alone, about 58 million people have them. And yet, many wait months - or years - before getting them checked. By then, the damage may have spread beyond what’s visible.
What Exactly Is an Actinic Keratosis?
An actinic keratosis (AK) is a patch of abnormal skin cells caused by years of sun exposure. It’s not a rash. It’s not just aging. It’s a warning sign. These lesions form in the top layer of the skin, the epidermis, where UV radiation has damaged the DNA in skin cells. Over time, those damaged cells don’t die off like they should. Instead, they multiply abnormally, creating rough, scaly patches. You won’t always see them. That’s why so many people miss them. AKs are often more noticeable by touch than by sight. Run your fingers over your forehead, nose, or the back of your hands. If you feel something gritty - like sandpaper - that’s a classic sign. The texture comes before the color. They can be red, pink, brown, gray, or even skin-colored. In people with darker skin, they often look like dark spots that don’t fade. The size varies. Most are between 1 and 2 centimeters, but some grow larger. A few develop into horn-like bumps, called hyperkeratotic AKs, which are a stronger signal that cancer could be forming. They show up where the sun hits hardest: face, scalp (especially in bald men), ears, neck, forearms, and the backs of hands. Nearly 85% of cases appear on the face or scalp.Why You Shouldn’t Ignore Them
Here’s the hard truth: actinic keratoses aren’t harmless. They’re precancers. That means they have the potential to become squamous cell carcinoma (SCC), the second most common type of skin cancer. About 10 to 15% of people with more than 10 AKs will develop SCC at some point. And here’s what most people don’t know - 90% of all SCCs start as untreated AKs. The risk isn’t the same for everyone. If you’re immunosuppressed - due to organ transplant, chemotherapy, or autoimmune disease - your chance of progression jumps to 25%. Even for healthy people, about 5 to 10% of individual AKs turn cancerous over 10 years. That might sound low, but when you have 15 or 20 lesions, the odds stack up. Doctors now treat AKs as early skin cancer. Dr. Henry W. Lim from Henry Ford Health System puts it simply: “Treating AKs is treating early skin cancer.” The goal isn’t just to remove a rough patch. It’s to stop cancer before it invades deeper layers of the skin.How Are They Diagnosed?
Most dermatologists can spot an AK with a quick visual and tactile exam. In fact, board-certified dermatologists diagnose them correctly 95% of the time just by looking and feeling. No biopsy is needed unless the lesion is unusually thick, tender, bleeding, or growing fast. Dermatoscopy - a handheld magnifying tool with polarized light - helps confirm the diagnosis. It reveals patterns invisible to the naked eye, like irregular blood vessels or white scales. But even without fancy tools, you can be your own first line of defense. A 2023 study from the Skin Cancer Foundation found that 78% of AKs are first noticed by patients themselves, usually because they feel something odd during daily routines - like shaving or washing their face. If a lesion looks suspicious - say, it’s raised over half a centimeter, ulcerated, or changing quickly - a biopsy is done. That’s not because it’s definitely cancer. It’s to rule out early SCC, which can look almost identical to a high-grade AK.
Field Treatment: The Game-Changer
Here’s the big shift in how AKs are treated today. In the past, doctors removed each lesion one by one with freezing (cryotherapy) or scraping. That worked for a few spots. But if you have 10, 15, or 20 lesions - and you’re likely to have dozens more that aren’t visible yet - that approach misses the real problem. The real problem is field cancerization. That’s when UV damage has spread across a large area of skin, even if no lesions are visible. Think of it like a lawn with weeds. You can pull up the visible ones, but if the soil is still full of seeds, more will grow. Field treatments target the entire damaged area - not just the obvious bumps. There are three main types of field treatments:- Topical medications: Creams or gels applied directly to the skin. These include 5% fluorouracil (5-FU), imiquimod, tirbanibulin, and ingenol mebutate.
- Chemical peels: Trichloroacetic acid (TCA) is used to remove the top layer of damaged skin. It’s fast, effective, and often done in the office.
- Photodynamic therapy (PDT): A light-sensitive solution is applied to the skin, then activated by a special light. This kills abnormal cells while sparing healthy ones.
What Do the Treatments Actually Do?
Each treatment works differently - and has different side effects. 5% Fluorouracil (5-FU) is the oldest and cheapest option. It’s a chemotherapy cream that stops abnormal cells from dividing. You apply it once or twice a day for 2 to 4 weeks. During that time, your skin gets red, swollen, crusty, and burns. It’s intense. But that’s the point - the inflammation means it’s working. Studies show 75 to 85% of lesions clear up. And here’s the kicker: it reduces new SCCs by up to 50% over five years. Imiquimod works by boosting your immune system to attack the bad cells. You apply it three times a week for up to 16 weeks. The side effects are milder than 5-FU, but the treatment takes longer. Clearance rates are around 54 to 75%. Tirbanibulin (Klisyri) is the newest. It’s a 5-day treatment - just apply it once a day for five days. It’s especially good for the face. It clears 44% of lesions completely. It’s expensive - about $650 per course - but it’s much more tolerable than 5-FU. Dermatologists now prefer it for facial AKs because patients stick with it. Ingenol mebutate is applied for 2 to 3 days. It causes rapid skin cell death. It’s effective but can cause severe irritation. It’s also one of the few treatments proven to reduce SCC development long-term. Photodynamic therapy involves applying a solution called aminolevulinic acid, waiting a few hours, then shining a blue or red light on the skin. It’s done in the clinic. One or two sessions are usually enough. Clearing rates are 44 to 75%. It’s less irritating than creams, but it’s more expensive and requires a light source.Choosing the Right Treatment
There’s no one-size-fits-all. Your choice depends on:- Where the lesions are (face? scalp? hands?)
- How many you have
- Your tolerance for side effects
- Your budget and insurance coverage
- Your lifestyle
- If you have 15 lesions on your forehead and want a quick fix, tirbanibulin is ideal.
- If you’re on a budget and don’t mind a few weeks of redness, 5-FU is still the gold standard.
- If you have AKs on your scalp and can’t apply cream easily, PDT might be better.
- If you’re older and have only a few low-grade spots, some doctors may suggest watching them instead of treating.


AKs aren’t ‘rough patches’-they’re DNA bombs ticking under your skin. 5-FU burns? Good. That’s the chemo doing its job. Ignore it, and you’re gambling with SCC. No sympathy for lazy sun-worshippers.
One must contemplate the ontological weight of photodamage: is the skin not merely a canvas, but a ledger of solar transgressions? The clinical paradigm, while efficacious, fails to address the metaphysical erosion wrought by ultraviolet entropy.
Let me tell you something, folks-America’s got the highest skin cancer rates because people think SPF 15 on a cloudy day is ‘enough.’ Nah. You need a damn tinfoil hat and a UV-blocking poncho. And if you’re not using 5-FU like it’s your job? You’re part of the problem.
Field treatment isn’t optional-it’s foundational. If you’ve got sun damage, you’ve got field cancerization. Period. The idea that you can just freeze one spot and call it quits is outdated. We need systemic thinking, not patchwork fixes. Everyone deserves access to PDT and topical regimens, regardless of income.
Let’s be real: 5-FU is a medieval torture device disguised as medicine. Tirbanibulin? $650? That’s a luxury SKU for the 1%. Meanwhile, I’ve got 17 AKs on my scalp and a 9-to-5. Who’s gonna pay for this? The system is rigged.
For anyone on the fence: if you feel sandpaper on your forehead, don’t wait. Get it checked. Dermatologists aren’t just selling creams-they’re stopping cancer before it whispers. And yes, the side effects suck. But so does chemo for SCC. Pick your pain.
ak? just let it be bro. sun dont kill u. its all hype. i got 20 yrs in arizona and still walkin. no cream nothin. chill.
My mom did 5-FU last year. She cried every night. But now her skin looks 10 years younger. Worth every second of hell.
Just a quick note for anyone starting treatment-don’t panic when your skin looks like a war zone. That redness? That’s your immune system waking up. Use aloe vera, keep it cool, and stick with it. You’re not just treating a patch-you’re protecting your future self. And if you’re overwhelmed? Talk to your derm. They’ve seen it all. You’ve got this.