
Bronchodilator Comparison Tool
Select Inhalers to Compare
Comparison Results
| Feature | ||||
|---|---|---|---|---|
| Mechanism | ||||
| Onset (min) | ||||
| Duration (h) | ||||
| Formulation | ||||
| Typical Rescue Dose |
If you’ve ever reached for an inhaler during an asthma flare, you probably know the brand name Asthalin. But how does it stack up against other rescue or maintenance inhalers? This guide breaks down the science, dosing, and real‑world pros and cons so you can decide which option fits your breathing needs.
What is Asthalin (Salbutamol)?
Asthalin (Salbutamol) is a short‑acting beta‑2 agonist (SABA) inhaler approved for rapid relief of bronchospasm in asthma and chronic obstructive pulmonary disease (COPD). Marketed in many countries under names like Ventolin or Proventil, its generic name is salbutamol. First launched in the 1970s, it quickly became a cornerstone of rescue therapy because it relaxes airway smooth muscle within minutes.
How Salbutamol Works as a Bronchodilator
Salbutamol binds to beta‑2 adrenergic receptors on airway smooth muscle cells. This triggers a cascade that increases cyclic AMP, which in turn inhibits calcium influx-essentially telling the muscle to relax. The result is a widened airway that lets air flow more freely. Because it targets receptors that are abundant in the lungs but sparse elsewhere, systemic side effects are relatively low when used as directed.
Key Alternatives to Asthalin
While Asthalin delivers quick relief, clinicians often pair or replace it with other agents depending on severity, frequency of symptoms, or patient preference. Below are the most common alternatives:
- Ventolin (Albuterol) - Another SABA with virtually identical pharmacology but marketed primarily in the United States.
- Atrovent (Ipratropium bromide) - A short‑acting anticholinergic that blocks muscarinic receptors, offering a different mechanism of bronchodilation.
- Symbicort (Budesonide/Formoterol) - A combination inhaled corticosteroid (ICS) with a long‑acting beta‑2 agonist (LABA), used for both control and quick relief in some protocols.
- Advair (Fluticasone/Salmeterol) - An ICS/LABA combo meant for maintenance, but its long‑acting component can supplement rescue therapy.
- QVar (Formoterol) - A LABA that has a relatively rapid onset (within 5 minutes) and can be used as a rescue inhaler in some regions.

Head‑to‑Head Comparison Table
| Brand (Generic) | Mechanism | Onset (min) | Duration (h) | Formulation | Typical Rescue Dose |
|---|---|---|---|---|---|
| Asthalin (Salbutamol) | Beta‑2 agonist | 1‑3 | 4‑6 | MDI (100 µg/puff) | 1‑2 puffs as needed |
| Ventolin (Albuterol) | Beta‑2 agonist | 1‑3 | 4‑6 | MDI (90‑100 µg/puff) | 1‑2 puffs |
| Atrovent (Ipratropium) | Anticholinergic | 5‑15 | 4‑6 | MDI (20 µg/puff) | 2 puffs |
| Symbicort (Budesonide/Formoterol) | ICS + LABA | ~5 (formoterol) | 12‑24 | MDI (80 µg/100 µg) | 1-2 puffs (as directed) |
| Advair (Fluticasone/Salmeterol) | ICS + LABA | ~10 (salmeterol) | 12‑24 | MDI (250 µg/50 µg) | Not a rescue inhaler |
When to Choose Asthalin vs. Alternatives
Both Asthalin and Ventolin are essentially interchangeable SABA options. Choose Asthalin if you’re in a region where the brand is readily available or covered by insurance. If you need a different inhaler device (e.g., a dry‑powder inhaler), consider a LABA like formoterol that can double as a rescue inhaler.
Anticholinergics such as Atrovent are valuable for patients who experience tachycardia or tremor from beta‑agonists, or for COPD patients where the cholinergic pathway plays a bigger role. In practice, many clinicians prescribe a SABA + anticholinergic combo for severe exacerbations.
Combination inhalers (Symbicort, Advair) are primarily for maintenance, but in some guidelines (e.g., GINA 2023) high‑dose formoterol can serve as a rescue agent, reducing the need for a separate SABA.
Potential Side Effects and Safety Considerations
SABAs are generally safe when used as directed, but overuse (more than 8 puffs per day) can lead to:
- Tremor
- Palpitations
- Low potassium (hypokalemia)
- Paradoxical bronchospasm (rare)
Anticholinergics can cause dry mouth, cough, or blurred vision, especially in older adults. Combination inhalers carry the usual steroid‑related concerns-hoarseness, oral thrush, and, with long‑term high doses, potential systemic effects.
Always rinse your mouth after using an inhaled corticosteroid and keep a rescue inhaler handy. If you notice persistent side effects, discuss dosage adjustments with your provider.
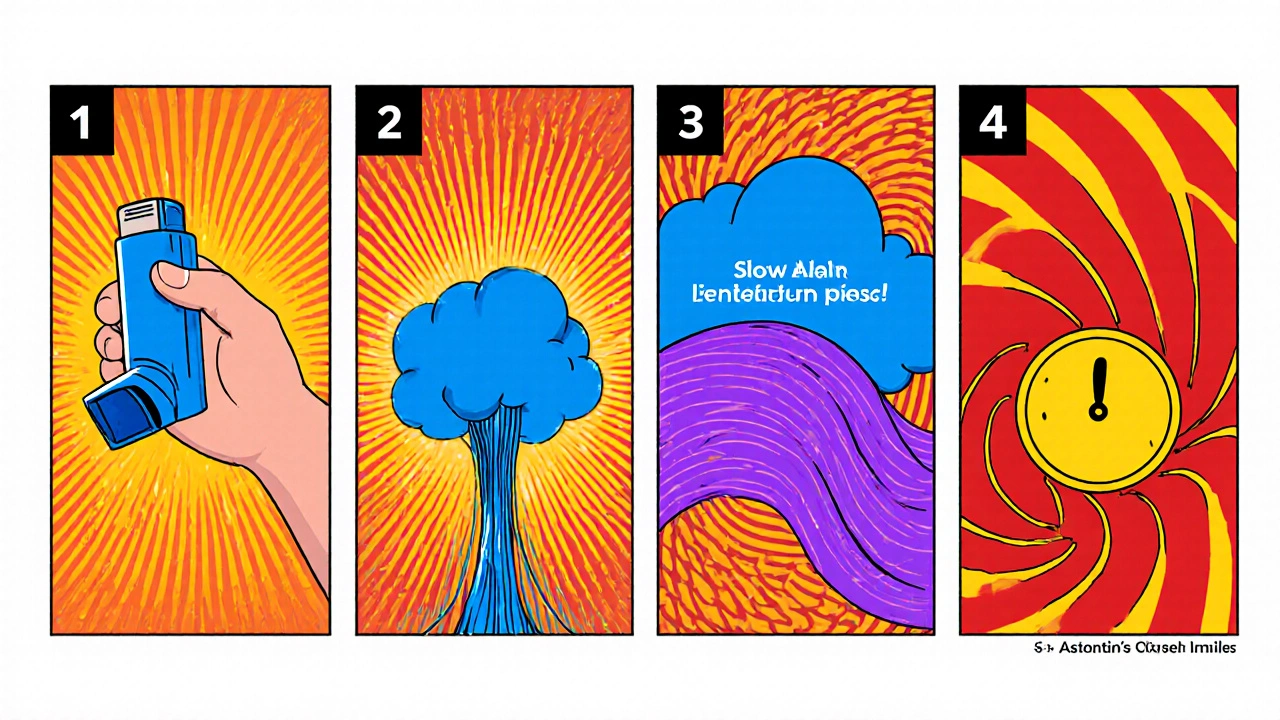
Tips for Using Inhalers Effectively
- Shake the MDI (like Asthalin) for at least 5 seconds before each use.
- Exhale fully, place the mouthpiece, then inhale slowly while actuating the device.
- Hold your breath for about 10 seconds to allow the medication to settle.
- Wait 30-60 seconds between puffs if you need a second dose.
- Store inhalers at room temperature, away from direct heat.
Following these steps maximizes drug delivery and reduces waste, making any inhaler-whether Asthalin or a comparator-more effective.
Quick Takeaways
- Asthalin (Salbutamol) offers the fastest onset (1‑3 min) among SABAs.
- Ventolin is pharmacologically identical; choose based on availability.
- Atrovent provides a non‑beta route, useful for COPD or beta‑agonist intolerance.
- Combination inhalers add anti‑inflammatory control but aren’t primary rescue options.
- Proper inhaler technique is as vital as the drug choice.
Can I use Asthalin and Ventolin interchangeably?
Yes. Both contain the same active ingredient (salbutamol/albuterol) and work the same way. The decision usually hinges on brand availability, insurance coverage, or device preference.
When should I add an anticholinergic like Atrovent to my regimen?
If you have frequent nighttime symptoms, COPD, or experience side effects (e.g., tremor) from SABAs, adding Atrovent can provide complementary bronchodilation without increasing beta‑agonist load.
Is it safe to use a combination inhaler like Symbicort for rescue?
In some guidelines, a high‑dose formoterol component can be used for quick relief, but you still need a SABA for immediate action. Always follow your doctor’s prescription and avoid exceeding recommended doses.
What are the warning signs of overusing Asthalin?
Symptoms include persistent tremor, rapid heartbeat, nervousness, and worsening asthma control despite frequent use. If you notice these, seek medical advice promptly.
How often should I replace my Asthalin inhaler?
MDIs typically contain 200 puffs. Replace the inhaler when you reach the low‑dose indicator (often a red line) or after 12 months, whichever comes first, even if doses remain.


Oh, the drama of choosing an inhaler-like picking a wand in a wizard's shop, but with far more at stake. Asthalin may be the "classic" you hear about in grandpa's stories, yet many modern patients overlook the subtle art of technique.
Allow me to elucidate the nuanced hierarchy of bronchodilators, beginning with the ostensibly humble Asthalin.
While the layperson may extol its rapid onset as a miracle, seasoned clinicians recognize that pharmacologically it is indistinguishable from its American counterpart, Ventolin.
Thus, the branding exercise serves merely as a marketing veneer rather than a therapeutic advancement.
Moreover, the anticholinergic alternative Atrovent, despite a slower onset, offers a commendable safety profile for beta‑agonist‑intolerant individuals.
One must not overlook the strategic value of combination inhalers such as Symbicort, which, when employed per guideline, can double as a rescue agent, albeit with the caveat of chronic steroid exposure.
The decision matrix, therefore, extends beyond onset and duration to encompass patient adherence, device familiarity, and insurance formularies.
Consider, for instance, a patient with limited dexterity who may struggle with the metered‑dose inhaler mechanism, rendering a dry‑powder inhaler a superior choice.
In contrast, the sleek aerodynamics of an MDI ensure rapid deposition in the peripheral airways, a factor that cannot be dismissed lightly.
It is also imperative to acknowledge the risk of tachyphylaxis associated with overuse of short‑acting beta‑agonists, a phenomenon that frequently precipitates emergency department visits.
Consequently, clinicians should counsel patients to limit rescue inhaler usage to no more than two puffs per episode and no more than eight puffs per day.
When the threshold is breached, a step‑up in controller therapy, perhaps incorporating an inhaled corticosteroid, becomes clinically justified.
Furthermore, the pharmacokinetic profile of formoterol, a rapid‑onset LABA, challenges the conventional dichotomy between SABA and LABA categories.
Indeed, some contemporary guidelines endorse the use of high‑dose formoterol as a sole rescue medication, a recommendation that certainly raises eyebrows among traditionalists.
Nevertheless, the overarching principle remains unchanged: optimal asthma management hinges upon personalized therapy, meticulous technique, and regular follow‑up.
In sum, Asthalin is neither a panacea nor an antiquated relic; it occupies a legitimate niche within a broader therapeutic arsenal, provided it is wielded judiciously.
Wow, that's a lot of info-so many layers! I guess the key takeaway is that every inhaler’s like a tiny philosophy of breathing, you know? If you treat the device with respect and keep the technique solid, the meds will do their magic. Stay hopeful and keep experimenting with what fits your lifestyle best. Remember, even a small typo in your routine can lead to big breakthroughs.
Asthalin's ubiquity renders it a textbook example of pharmaceutical complacency.
For patients transitioning between devices, a step‑by‑step walkthrough can make all the difference-start with a demonstration, then let them practice under supervision, and finally verify proper inhalation technique.
Seriously, stop sugar‑coating the pain of poor technique; if you can't handle a simple shake, you deserve the extra coaching, not a free ride.
The clinical tableau of bronchodilator choices is a kaleidoscope of mechanisms-each hue shimmering with potential, each shadow hinting at side‑effects.
Remember, the most effective inhaler is the one you actually use correctly; consistent education and gentle reminders foster lasting mastery.
When comparing onset times, keep in mind that Salbutamol and Albuterol both reach peak effect within 1‑3 minutes, whereas Ipratropium lags behind at 5‑15 minutes, which can be crucial during a sudden nocturnal attack.
In practice, pairing a SABA with an anticholinergic can provide synergistic relief without doubling beta‑agonist exposure.
Your tip about pairing is spot on-I've seen patients breathe easier when we add a puff of Atrovent after the usual two puffs of Asthalin.
Stick to the 10‑second breath‑hold; it maximizes deposition.
Even if you feel uneasy about frequent inhaler use, trust the data: staying within recommended limits prevents tolerance and keeps your lungs responsive.
It is a common misconception that occasional overuse of a rescue inhaler signals a failure of one's character rather than a physiological cue; in reality, the body is simply signaling that maintenance therapy may need adjustment.
By reviewing peak flow trends and symptom diaries, clinicians can fine‑tune the regimen, perhaps introducing a low‑dose inhaled corticosteroid to curb inflammation.
Such proactive measures often eliminate the reliance on multiple puffs per day, preserving both lung function and quality of life.
Ultimately, a collaborative partnership between patient and provider, grounded in honest communication, yields the most sustainable outcomes.
Don't be fooled by the pharmaceutical narrative that all SABAs are created equal; hidden formularies manipulate dosing standards to keep patients dependent on brand‑specific refills.
This is why sticking to a single, trusted inhaler saves you from the hidden agenda.