
Suicidal Ideation Risk Assessment Tool
This tool helps identify warning signs associated with depressive disorder and suicidal thoughts. It is not a substitute for professional diagnosis. If you or someone you know is in crisis, please contact emergency services immediately.
When we talk about depressive disorder is a mental health condition marked by persistent low mood, loss of interest, and a range of physical and emotional symptoms that last at least two weeks, the risk of developing Suicidal Thoughts-also known as suicidal ideation-increases dramatically. If you or someone you know is dealing with both, you’re probably wondering why these two often travel together and what you can do about it.
Why Do Depressive Episodes Trigger Suicidal Ideation?
There isn’t a single magic bullet that explains the link; instead, several biological, psychological, and social pieces fit together like a puzzle.
Neurobiology: The Serotonin Connection
Research published by the National Institute of Mental Health in 2023 shows that people with major depressive episodes often have lower levels of serotonin-a neurotransmitter that helps regulate mood, impulse control, and pain perception. When serotonin drops, the brain’s ability to suppress negative thoughts weakens, making thoughts of suicide feel more attainable.
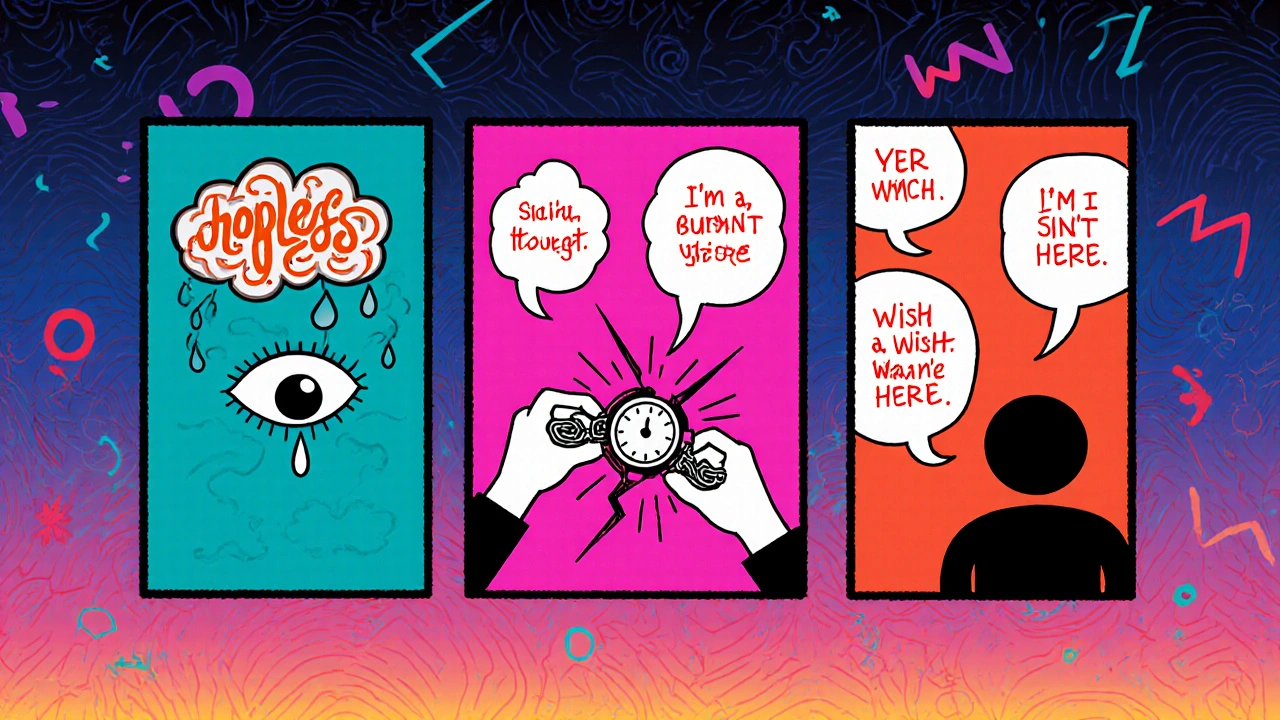
Psychological Factors: Hopelessness and Rumination
Two mental habits stand out:
- Hopelessness: Feeling that the future will never improve. A longitudinal study of 2,000 adults found that hopelessness doubled the odds of experiencing suicidal thoughts within six months.
- Rumination: Repetitive, negative self‑talk that traps a person in a cycle of blame. When rumination intensifies, the mind often searches for an escape, and suicide can appear as a fast‑acting solution.
Social Triggers: Isolation and Stress
Loneliness, job loss, or relationship breakdowns push a vulnerable brain over the edge. A 2022 survey of 1.5 million U.S. adults revealed that people who reported high social isolation were three times more likely to endorse suicidal thoughts during a depressive episode.
Key Warning Signs to Watch For
Being able to spot the red flags early can save a life. Below is a quick‑reference table that groups emotional, behavioral, and verbal cues.
| Category | Specific Signs | Why It Matters |
|---|---|---|
| Emotional | Intense hopelessness, sudden calm after a period of agitation | Signals a shift from thinking about suicide to planning |
| Behavioral | Withdrawing from friends, giving away prized items, risky substance use | Acts can be preparation steps for a final act |
| Verbal | Talking about death as a solution, "I’m a burden", "I wish I wasn’t here" | Direct language often precedes a crisis |
How Professionals Assess the Risk
Screening tools help clinicians gauge severity and decide on immediate action.
- PHQ‑9 - A nine‑item questionnaire that includes a specific question about thoughts of death or self‑harm. Scores of 10 or higher usually indicate moderate to severe depression and warrant a deeper risk assessment.
- Columbia Suicide Severity Rating Scale (C‑SSRS) - Offers a step‑by‑step probe of suicidal thoughts, plans, and intent. It’s widely used in emergency rooms and crisis hotlines.
Clinicians combine these scores with a clinical interview, paying close attention to the timeline of depressive symptoms and any recent life stressors.
Prevention and Intervention Strategies
Knowing the link is only half the battle. Below are evidence‑based actions that can turn the tide.
Therapeutic Approaches
- Cognitive Behavioral Therapy (CBT) - Teaches patients to challenge hopeless thoughts and replace them with realistic alternatives. A meta‑analysis of 30 studies showed CBT reduces suicidal ideation by 31% compared with control groups.
- Dialectical Behavior Therapy (DBT) - Specifically targets emotional dysregulation and self‑harm behaviors. DBT’s “distress tolerance” skills have been linked to lower suicide attempts.
Medication Management
Selective serotonin reuptake inhibitors (SSRIs) are the first‑line pharmacological treatment for depressive disorder. While SSRIs can initially increase agitation for a small subset of patients, careful monitoring during the first 2‑4 weeks dramatically reduces long‑term suicide risk.
Safety Planning and Crisis Resources
Creating a written safety plan-listing coping strategies, supportive contacts, and emergency numbers-has been shown to cut repeat suicide attempts by up to 40%.
In the U.S., dialing 988 connects callers to the Suicide and Crisis Lifeline, a free, 24‑hour service staffed by trained counselors.
Common Myths About Depression and Suicide
Debunking misconceptions helps reduce stigma and encourages help‑seeking.
- Myth: "Only "crazy" people think about suicide." Reality: Over 90% of people who die by suicide have a diagnosable mental health condition, most often depression. \n
- Myth: "Talking about suicide gives someone the idea." Reality: Open conversation often provides relief and a sense of being heard, which can be protective.
- Myth: "If they don’t have a plan, they’re safe." Reality: Thoughts can quickly evolve into plans; early intervention is key.

Quick Checklist for Friends and Family
- Notice any sudden mood shift or calm after a period of agitation?
- Listen without judgment if they mention death, hopelessness, or being a burden.
- Ask directly: "Are you thinking about harming yourself?"
- Stay with them or arrange safe supervision until professional help arrives.
- Encourage a mental‑health appointment and offer to accompany them.
Frequently Asked Questions
Can someone be on medication for depression and still have suicidal thoughts?
Yes. Medications, especially during the first weeks, can sometimes increase anxiety or agitation. That’s why clinicians monitor patients closely and adjust dosages if needed.
Is it safe to ask a depressed person directly about suicide?
Absolutely. Direct, non‑judgmental questions often open a dialogue and give the person a chance to share their feelings. Phrase it simply: "Are you having thoughts of harming yourself?"
What’s the difference between suicidal thoughts and a suicide plan?
Thoughts are vague ideas about death or self‑harm. A plan includes specific details like method, timing, or location. A plan indicates higher risk and needs immediate professional intervention.
How quickly can therapy reduce suicidal ideation?
Evidence‑based therapies such as CBT can show measurable reductions in suicidal thoughts within 6‑8 weeks. The timeline varies, but early engagement is critical.
Are there any warning signs that don’t involve talking about death?
Yes. Sudden calm after a period of agitation, giving away personal belongings, or taking “final” actions (e.g., writing a goodbye note) can be silent alarm bells.
Understanding the connection between depressive disorder and suicidal thoughts is a crucial step toward prevention. By recognizing the signs, using proper assessment tools, and acting quickly with therapy, medication, and safety plans, families, friends, and clinicians can make a real difference. If you suspect someone is at risk, reach out now-there’s always help on the other side of the call.


America's mental health crisis is just another excuse for the media to push their leftist agenda!! The so‑called "depressive disorder" link to suicidal thoughts is overhyped, and the government uses it to control folks.
It's all a part of the grand scheme to keep the population scared and obedient, orchestrated by unseen forces.
Oh my gosh!!! This is like a drama straight out of a tragic soap opera!! The world is a stage and we are the helpless actors caught in the spotlight of despair!!!
One might contemplate the existential tether that binds melancholy to the abyss; indeed, the human psyche, when submerged in the chiaroscuro of hopelessness, often contemplates the finale as a paradoxical emancipation.
Understanding the intricate relationship between depressive disorder and suicidal ideation is a vital step toward fostering hope and resilience.
Research consistently shows that early intervention, whether through evidence‑based therapies like CBT or DBT, can significantly diminish the intensity of hopeless thoughts.
Moreover, the neurobiological insights into serotonin deficits remind us that medication, when carefully monitored, provides a crucial neurochemical foundation for recovery.
It's essential for friends and family to recognize subtle warning signs such as sudden calm after agitation, as these can signal a transition from rumination to planning.
Open, non‑judgmental conversations about feelings of burden or death are not dangerous; they actually create a safety net for the individual.
Safety planning, involving written strategies and emergency contacts, has been demonstrated to reduce repeat attempts by a substantial margin.
Professional tools like the PHQ‑9 and C‑SSRS equip clinicians with objective data to gauge risk and tailor treatment.
In the United States, the Suicide and Crisis Lifeline (988) offers immediate support, underscoring the importance of accessible resources.
Stigma reduction through myth‑busting-recognizing that suicidal thoughts are not exclusive to “crazy” people but closely linked to mental illness-encourages help‑seeking behavior.
Encouraging optimism and emphasizing that depressive episodes are treatable can empower individuals to pursue therapy and medication adherence.
Community initiatives that combat isolation, such as support groups and outreach programs, further buffer against the social triggers of despair.
While the path to recovery may be non‑linear, consistent engagement with mental‑health professionals fosters resilience.
Each small step-whether a coping skill from DBT or a moment of honest disclosure-builds momentum toward healing.
Remember, the presence of a supportive network dramatically improves outcomes, reinforcing the truth that no one needs to face these battles alone.
In sum, integrating scientific knowledge, compassionate communication, and timely interventions creates a roadmap for saving lives and restoring hope 😊.
Oh sure, because a 15‑sentence pep talk is exactly what someone in crisis needs-maybe next they’ll want a dissertation on quantum mechanics to feel better.
From an academic perspective, the correlation between depressive pathology and suicidal cognition warrants a nuanced discourse, yet the lay public often conflates correlation with causation, thereby oversimplifying a complex psychosocial phenomenon.
Let’s channel that scholarly insight into actionable compassion! By blending vibrant community outreach with evidence‑based interventions, we can turn the tide of despair into a wave of collective resilience. 🌊✨