
Smoking Risk Assessment Tool
How Smoking Affects Your Oral Health
Enter your smoking habits to see personalized risk assessment and recovery timeline.
Ever wonder why your dentist keeps warning you about cigarettes? The truth is, effects of smoking on teeth go far beyond a yellow stain. In this guide we’ll break down exactly how tobacco messes with the mouth, what that means for your smile, and practical steps you can take whether you’re a long‑time smoker or just thinking about quitting.
What "Smoking" Really Does Inside Your Mouth
Smoking is a habit that forces nicotine, carbon monoxide, and hundreds of other chemicals into the oral cavity. Those toxins coat every surface, shrink blood vessels, and blunt the cells that normally repair tissue. The result? A perfect storm that attacks both hard and soft oral structures.
Understanding "Oral Health" and Why It Matters
Oral health refers to the condition of the teeth, gums, tongue, and the entire mouth. Good oral health isn’t just about a bright smile; it’s linked to heart disease, diabetes, and even pregnancy outcomes. When smoking enters the equation, the whole system takes a hit.
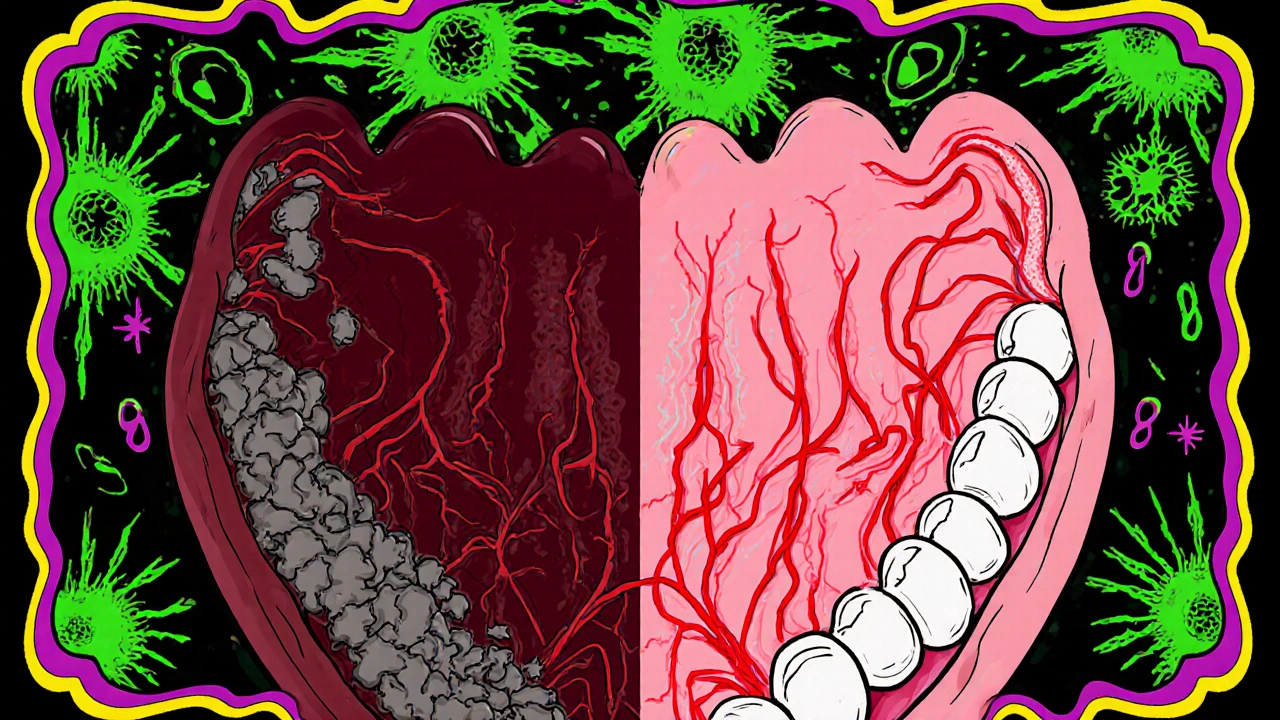
How Smoking Attacks Your Teeth
First up, the hard part of your mouth-your Teeth are the calcified structures that bite, chew, and speak. Tobacco’s acidic byproducts erode enamel, the protective outer layer. Once enamel wears down, you’re left with increased sensitivity and a higher chance of cavities. Moreover, nicotine reduces saliva flow, which means less natural rinsing of food particles and acids.
- Enamel erosion speeds up by up to 30% in heavy smokers.
- Dry mouth (xerostomia) appears in about 40% of daily smokers.
- Visible brown or gray stains develop within weeks of regular use.
The Toll on Your Gums
Your Gums are the soft tissue that surrounds and supports the teeth rely on a steady blood supply to stay healthy. Smoking narrows the tiny blood vessels, starving the gums of oxygen and nutrients. This makes them more prone to inflammation and infection.
One of the most serious gum conditions linked to smoking is Periodontitis a chronic inflammatory disease that destroys the bone and ligament holding teeth in place. Studies show smokers are 2-6 times more likely to develop periodontitis than non‑smokers, and the disease progresses faster.
Dental Plaque, Tartar, and the Smoking Connection
Even the tiny biofilm you can see on a brush-Dental plaque a sticky collection of bacteria, food particles, and saliva-gets a boost from tobacco. The chemicals change the bacterial mix, encouraging aggressive strains that produce more acid.
When plaque calcifies, it becomes Tartar a hard deposit that can only be removed by a dentist or hygienist. Smoking accelerates this hardening, so you’ll need professional cleanings more often.
Bad Breath (Halitosis) and Stubborn Stains
Ever notice that lingering “cigarette smell” after a smoke? That’s Halitosis persistent bad breath caused by oral bacteria and external odors. The reduced saliva flow and altered bacterial environment give the odor a longer lifespan.
Stains aren’t just cosmetic; they’re a visual reminder of the chemicals embedding themselves in enamel. While professional whitening can lift some of the discoloration, the underlying damage remains until you quit.
Smoking and Oral Cancer Risk
Perhaps the scariest statistic: smokers are up to 13 times more likely to develop Oral cancer malignant tumors that can appear on the lips, tongue, cheeks, floor of the mouth, and throat. The culprit is not just nicotine but the mix of carcinogens like nitrosamines and benzopyrene that linger in the mouth after each puff.
Early signs-white or red patches, persistent soreness, or a lump that won’t go away-often get missed because they’re confused with common gum irritation. Regular dental exams are crucial for catching these changes early.
What Happens When You Quit Smoking?
The good news is that your mouth starts to heal within days. Blood flow improves, saliva production normalizes, and the immune system regains strength. Here’s a quick timeline:
- 24‑48 hours: Breath smells fresher; temperature of the mouth stabilizes.
- 2‑4 weeks: Gums regain some of their pink color; plaque buildup slows.
- 3‑6 months: Cilia in the respiratory tract recover, reducing cough and dry mouth.
- 1‑2 years: Risk of periodontitis drops to near‑non‑smoker levels.
- 5+ years: Oral cancer risk halves compared to a continuing smoker.
Even if you’ve smoked for decades, the body can still bounce back, but the longer you stay tobacco‑free, the better the outcome.
Practical Steps to Protect Your Oral Health Right Now
If you’re not ready to quit, these habits can at least blunt the damage:
- Rinse after every cigarette: Use an alcohol‑free mouthwash with fluoride to neutralize acids.
- Stay hydrated: Drink water frequently to boost saliva.
- Boost oral hygiene: Brush twice a day with a soft‑bristle brush, floss daily, and consider an antibacterial toothpaste.
- Visit the dentist quarterly: More frequent cleanings catch plaque and tartar before they become a problem.
- Chew sugar‑free gum: Stimulates saliva and washes away leftover chemicals.
Combine these with a quit‑plan-nicotine replacement, counseling, or apps-and you’ll give your mouth the best chance to recover.
Quick Takeaways
- Smoking speeds up enamel erosion, dries out the mouth, and fuels plaque growth.
- Gum tissue suffers from reduced blood flow, leading to higher rates of periodontitis.
- Bad breath, stubborn stains, and a dramatically higher oral cancer risk are direct side‑effects.
- Healing begins within days of quitting, with major risk reductions after a year.
- Better oral hygiene, frequent dental visits, and staying hydrated can mitigate damage if quitting isn’t immediate.
Does vaping affect oral health the same way as smoking?
Vaping still delivers nicotine and propylene glycol, which can dry the mouth and alter bacterial balance. While it may cause less staining, the risk of gum inflammation and reduced saliva remains.
Can nicotine gum or patches still harm my teeth?
Nicotine replacement products avoid the combustion chemicals that damage enamel, but they still reduce saliva flow. Using them with plenty of water and good oral hygiene keeps the risk low.
How often should a smoker see the dentist?
At least every three months. More frequent cleanings catch plaque, tartar, and early gum disease before they become severe.
Is there a link between smoking and tooth loss?
Yes. The combination of faster enamel decay, aggressive gum disease, and reduced healing capacity makes smokers up to three times more likely to lose teeth prematurely.
What’s the best mouthwash for a smoker?
Look for alcohol‑free formulas with fluoride and antibacterial agents like cetylpyridinium chloride. They neutralize acids without further drying the mouth.


Man, the way smoking basically robs your gums of blood is like watching a drama unfold in slow motion. I mean, you light up, and your mouth’s blood supply does a nosedive, leaving your gums to wither. No wonder dentists shout about it. It’s a silent killer for your smile.
Statistically, smokers exhibit a 2‑6× higher incidence of periodontitis due to vasoconstriction in the gingival vasculature. The reduced perfusion also impairs fibroblast activity, slowing tissue repair.
It is an incontrovertible fact that the act of inhaling burned tobacco is one of the most egregious assaults on one's oral cavity ever documented in dental literature. First, the tar and nicotine cocktail coats every tooth surface, forming a tenacious pellicle that not only stains but also accelerates the demineralization of enamel. Second, the systemic vasoconstrictive effect of nicotine starves the gingival tissues of essential oxygen, rendering them incapable of mounting an effective inflammatory response. Third, the chronic dryness induced by reduced salivary flow eliminates the mouth's natural buffering capacity, allowing acidogenic bacteria to proliferate unchecked. Fourth, the altered microbiome favors pathogenic species such as Porphyromonas gingivalis, which are directly implicated in the pathogenesis of periodontitis. Fifth, the cumulative effect of these processes is a dramatically heightened risk of alveolar bone loss, ultimately leading to tooth mobility and loss. Sixth, let us not forget that the carcinogenic nitrosamines present in cigarette smoke confer a staggering increase-up to thirteenfold-in the probability of developing oral squamous cell carcinoma. Seventh, this oncogenic threat is compounded by the fact that early lesions often masquerade as benign gingival irritation, delaying diagnosis. Eighth, the psychological impact of discolored teeth and halitosis further erodes a person's self‑esteem, creating a feedback loop of stress that can exacerbate periodontal disease. Ninth, while some may argue that occasional smoking is benign, the dose‑response relationship is clear: even a few cigarettes per day initiate measurable changes in plaque composition. Tenth, the evidence is unequivocal that cessation triggers a cascade of reparative processes, beginning with restored blood flow within 24–48 hours. Eleventh, within weeks, gingival coloration improves, and the rate of plaque accumulation declines noticeably. Twelfth, after several months of abstinence, the risk of periodontitis approaches that of a lifelong non‑smoker, underscoring the plasticity of oral tissues. Thirteenth, consequently, dental professionals have an ethical imperative to counsel patients aggressively about these risks. Fourteenth, the societal cost of smoking‑related dental disease, in terms of both healthcare expenditure and lost productivity, is immeasurably high. Finally, the only truly responsible choice for anyone who values their oral health is to quit smoking outright.
Reading that thorough breakdown really puts things into perspective; it’s scary but also empowering. Knowing that the body can start healing within days gives hope to anyone thinking about quitting. Small steps like drinking water after each cigarette can make a noticeable difference. Keep sharing this info-it helps people take control of their health.
Great rundown, Ron. If you’re looking to quit, try swapping each cigarette for a short walk; the distraction combined with fresh air does wonders.
Honestly, only a fool would ignore the dental devastation smoking causes.
The epidemiological correlation between nicotine exposure and periodontal degeneration is well-established in peer‑reviewed studies. Consequently, dental prophylaxis protocols for smokers must be intensified to mitigate accelerated tissue loss. Adherence to such evidence‑based guidelines is a professional responsibility.
While the data you present is undeniably compelling, it's also crucial to consider patients' socioeconomic contexts, which often influence smoking prevalence, access to care, and compliance with treatment plans; therefore, a holistic approach that combines education, affordable cessation programs, and community support can bridge the gap between knowledge and action. Integrating these strategies into routine dental visits could dramatically reduce the burden of oral disease across populations.
I hear you on the need for broader support; many patients feel trapped by circumstances beyond their control. Offering low‑cost nicotine patches at the clinic might be a simple yet effective step.
Your exhaustive analysis aligns perfectly with current literature, and the statistical underpinnings are indisputable. 📊 The incremental risk multipliers you cite are supported by meta‑analyses spanning multiple demographics. 📈 Moreover, the temporal healing curve you outline underscores the resilience of periodontal tissues post‑cessation. 🦷 Finally, disseminating such comprehensive guidance on public platforms can catalyze behavioral change at scale. 🌐
Yo, that whole smoke‑kill mouth thing is straight up loco, man. You gotta ditch the buts and just quit, no more excuses. The gums gonna thank ya, trust.
One might argue that the dramatization of smoking's oral effects serves a broader agenda of fear‑mongering, yet the empirical evidence remains unassailable. Nevertheless, the discourse could benefit from a more nuanced examination of alternative nicotine delivery systems.