Many people turn to St. John’s Wort because it’s natural, affordable, and widely available. It’s often marketed as a safe alternative to antidepressants for mild depression. But here’s the truth: St. John’s Wort isn’t harmless. Even though it’s sold as a supplement, it acts like a powerful drug inside your body - and it can mess with prescription medications in ways that are dangerous, sometimes life-threatening.
How St. John’s Wort Changes How Your Body Handles Medications
St. John’s Wort doesn’t just float around in your system. It actively changes how your liver and gut process other drugs. The key player is a compound called hyperforin. Once you take it, hyperforin turns on enzymes - especially CYP3A4 and CYP2C9 - that break down medications faster. It also kicks up the activity of P-glycoprotein, a protein that pushes drugs out of your cells. Together, this means your body flushes out other medicines before they can do their job.
Studies show that after just two weeks of taking 900 mg of St. John’s Wort daily, these enzymes can become 40% more active. That’s not a small change. It can slash the blood levels of your prescription drugs by 30% to 50%. For some people, that’s the difference between a drug working and not working at all.
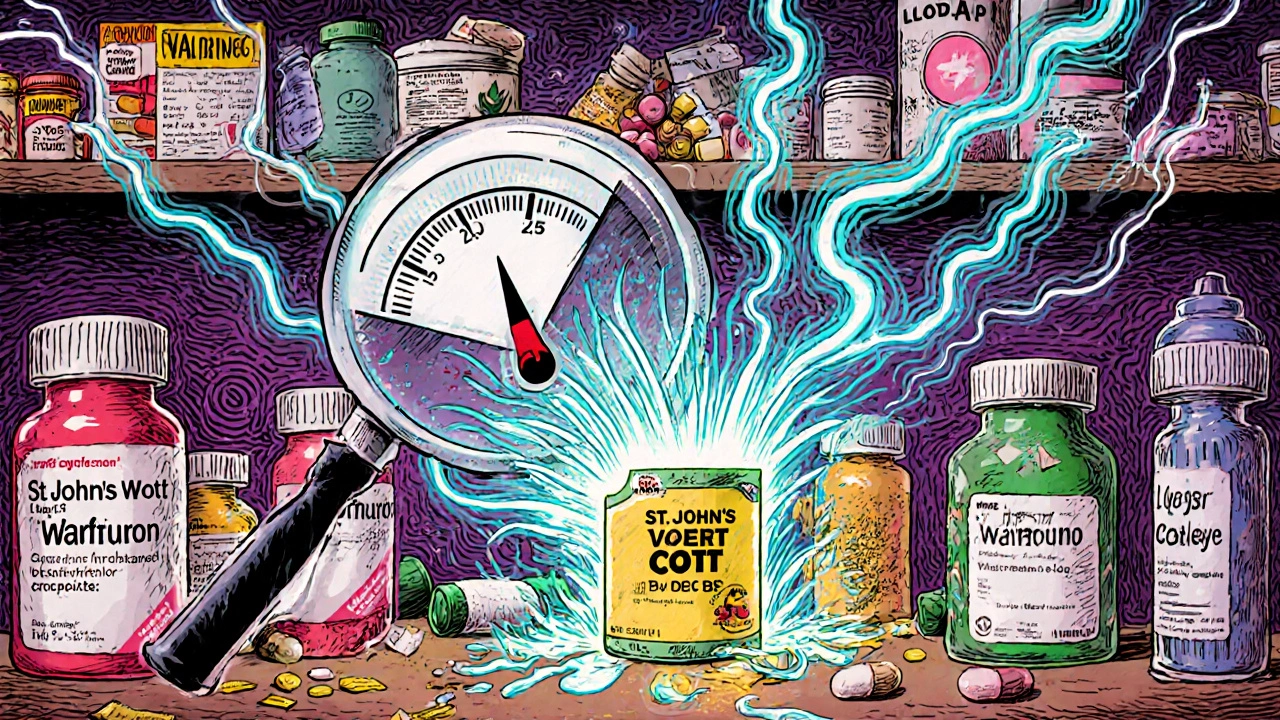
Warfarin: When Your Blood Thinner Stops Working
If you’re on warfarin to prevent blood clots, taking St. John’s Wort could put you at serious risk. Warfarin has a narrow safety window - too little and you clot; too much and you bleed. St. John’s Wort drops warfarin levels by about 25%. Documented cases show INR levels - a measure of blood clotting time - dropping from a safe 2.5 to a dangerous 1.3 in under a week. One patient in Australia had to have their warfarin dose increased by 25% just to get back to a stable level.
The Australian Therapeutic Goods Administration recorded 22 cases of unstable INR linked to St. John’s Wort between 1998 and 2000. These aren’t rare accidents. They’re predictable outcomes of a known interaction. And here’s the kicker: many patients didn’t even tell their doctor they were taking it.
Organ Transplant Rejection: A Silent Threat
People who’ve had organ transplants rely on immunosuppressants like cyclosporine or tacrolimus to keep their body from rejecting the new organ. These drugs need to stay at very precise levels in the blood. Too low, and rejection can happen fast - sometimes within days.
St. John’s Wort can drop cyclosporine levels by 30% to 50%. One transplant patient on HealthUnlocked reported his levels fell 40% after starting St. John’s Wort for depression. His doctor told him he was “hours away from organ rejection.” That’s not an exaggeration. In hospital settings, these kinds of interactions lead to emergency readmissions, extra testing, and sometimes the loss of the transplanted organ.
HIV Medications: Risking Treatment Failure
For people living with HIV, missing a single dose of antiretroviral drugs can lead to drug resistance. St. John’s Wort makes this risk even worse. It reduces the blood levels of key HIV medications - including protease inhibitors like saquinavir and non-nucleoside reverse transcriptase inhibitors like efavirenz - by up to 50%.
That means the virus isn’t fully suppressed. It mutates. It becomes resistant. And once that happens, fewer treatment options remain. The FDA and the Therapeutic Goods Administration both warn about this interaction. Yet, many patients still take St. John’s Wort without telling their HIV specialist, thinking it’s “just an herb.”
Antidepressants and Serotonin Syndrome: A Medical Emergency
St. John’s Wort doesn’t just interfere with other drugs - it acts like an antidepressant itself. It increases serotonin in the brain by blocking its reuptake, similar to SSRIs like sertraline or fluoxetine. That’s fine if you’re using it alone. But when you combine it with an SSRI, SNRI, or even the antidepressant nefazodone, serotonin levels can spike dangerously.
Serotonin syndrome is real. Symptoms include confusion, rapid heart rate, high blood pressure, muscle rigidity, fever, and seizures. In extreme cases, it can be fatal. The Australian TGA documented six cases of serotonin syndrome linked to St. John’s Wort combined with SSRIs. Symptoms appeared in 3 to 7 days. One patient had to be hospitalized. Another needed intensive care.
And here’s the scary part: many people don’t realize they’re combining the two. They start St. John’s Wort because they’re still feeling down on their antidepressant. They think, “More natural help can’t hurt.” But it can.
Birth Control, Statins, and Other Hidden Risks
St. John’s Wort doesn’t just affect brain or heart meds. It can break down birth control pills. Ethinyl estradiol, the main estrogen in most oral contraceptives, can drop by 25% to 35%. There are 13 documented cases of unintended pregnancy in women who took birth control perfectly - but also took St. John’s Wort. One user on Drugs.com wrote: “I had breakthrough bleeding, then found out I was pregnant.”
Statins aren’t all equal. Atorvastatin and simvastatin - the most common cholesterol drugs - are broken down by CYP3A4, so St. John’s Wort cuts their levels by 30% to 40%. That means your cholesterol isn’t being controlled. But pravastatin and fluvastatin? They’re metabolized differently. No major interaction. Still, most people don’t know the difference.
Other drugs at risk include:
- Benzodiazepines (like alprazolam/Xanax): 40% lower levels, so anxiety returns
- Anticonvulsants (phenytoin, carbamazepine): 30-40% reduction, risking seizures
- Digoxin: 25% drop, leading to heart failure
- Theophylline: 30% lower, worsening asthma
- Proton pump inhibitors (omeprazole): reduced effectiveness
- Opioids: lower pain relief, possible withdrawal
Why People Don’t Realize the Danger
Most people assume “natural” means “safe.” That’s the biggest myth. St. John’s Wort is sold in pharmacies, health stores, and online. Labels say “dietary supplement,” so many think it’s like taking vitamin C. But it’s not. It’s a potent biochemical agent.
A 2022 Johns Hopkins study found that 73% of patients who had interactions with St. John’s Wort didn’t know it could interfere with their meds. And 41% never told their doctor they were taking it. Why? Because they weren’t asked the right question.
Doctors often ask, “Are you taking any other medications?” But patients don’t think of supplements as medications. They say, “No.”
The right question is: “Do you take any herbal supplements, vitamins, or over-the-counter products?” That’s the one that gets the truth.
What You Should Do
If you’re taking any prescription drug, don’t start St. John’s Wort without talking to your doctor or pharmacist. Even if you’ve been taking it for months, tell them now. Don’t wait for a problem to happen.
If you’re already on it and want to stop, don’t quit cold turkey. Because enzyme induction doesn’t vanish the day you stop. It takes up to two weeks for your liver to return to normal. That means if you start a new medication right after stopping St. John’s Wort, it could build up to toxic levels - because your body isn’t breaking it down as fast anymore.
For critical drugs like warfarin, cyclosporine, or HIV meds, your provider should monitor levels before and after starting or stopping St. John’s Wort. INR checks, drug trough levels, and seizure thresholds need tracking.
And if you’re using it for depression - even mild - know this: the American Psychiatric Association’s 2023 guidelines no longer recommend it for anyone on prescription meds. The risks outweigh the benefits.
The Bottom Line
St. John’s Wort might help with low mood. But it’s not a gentle herb. It’s a drug that rewires how your body handles other drugs. It can make your blood thinner useless. It can cause your transplant to fail. It can trigger a seizure. It can get you pregnant on birth control. It can cause serotonin syndrome.
There’s no safe gray area. If you’re on any prescription medication, avoid St. John’s Wort. If you’re already using it, talk to your provider. Don’t assume it’s harmless because it’s natural. It’s not. And the consequences aren’t theoretical - they’re documented, real, and sometimes deadly.

Thank you for sharing this. I’ve seen too many people assume herbs are safe because they’re natural. My mom took St. John’s Wort with her blood pressure med and ended up in the ER. No one asked her about supplements. We all need to ask better questions.
Doctors need to change how they ask. Not ‘any medications?’ but ‘any vitamins, teas, or herbal pills?’ That’s the difference between life and a hospital visit.
Of course the FDA and TGA warn about it - they’re complicit in the pharmaceutical monopoly. St. John’s Wort has been used for centuries in Europe. The real danger is that Big Pharma doesn’t profit from it, so they’ve weaponized regulatory fear to suppress natural alternatives. This article reads like a paid ad for antidepressant manufacturers.
Hyperforin? CYP3A4? You’re speaking in coded corporate language. The truth is, they don’t want you to know you can heal yourself without a prescription.
While the pharmacokinetic mechanisms described are accurate, the tone of this post is alarmist and lacks nuance. The interaction profile of St. John’s Wort is well-documented in clinical pharmacology literature, and its effects are dose- and duration-dependent.
Moreover, the assertion that there is ‘no safe gray area’ is scientifically indefensible. Patients on stable, low-dose SSRIs with no comorbidities may tolerate low-dose hypericum under supervision. The blanket condemnation ignores individual risk stratification - a cornerstone of evidence-based medicine.
As a clinical pharmacist, I see this every week. Patients come in saying, ‘I started this tea for anxiety’ - and then their INR crashes or their transplant numbers drop. They don’t call it a drug. They call it ‘herbal support.’
We need standardized screening tools in EHRs. Not just a checkbox under ‘medications’ - but a forced dropdown with ‘St. John’s Wort’ listed explicitly. If it’s not on the list, it doesn’t get documented. That’s the reality.
So let me get this straight - you’re telling me that a plant that’s been used since ancient Greece is now suddenly a ‘life-threatening drug’ because some lab rats showed enzyme changes? Where’s the real-world mortality data? How many people have actually died from this? Not ‘INR dropped’ - I mean DEAD. Like, buried. Because of St. John’s Wort?
Meanwhile, SSRIs kill 10,000 people a year in the US alone. But nobody’s banning Prozac because it’s ‘natural.’ Funny how that works.
Of course they’re warning you about St. John’s Wort. It’s not about safety - it’s about control. The medical-industrial complex needs you dependent on monthly prescriptions. If you could fix depression with a $10 bottle of herbs from the corner store, why would they invest in therapy, psychiatrists, or mental health infrastructure?
They don’t want you to know that sunlight, exercise, and hypericum work better than fluoxetine for mild cases. That’s why they scare you with ‘enzyme induction’ and ‘trough levels.’ It’s not science - it’s fear marketing.
I’ve worked with transplant patients for over 15 years. One case still haunts me: a 32-year-old woman on tacrolimus. She started St. John’s Wort because she felt ‘down’ after surgery. She didn’t think it mattered. Two weeks later, her creatinine spiked. Biopsy showed acute rejection.
She lost her kidney. She’s on dialysis now. She didn’t know. No one asked. That’s the tragedy - not the herb. The silence.
I used to take St. John’s Wort for my anxiety. I thought it was gentle. Then I started feeling jittery, my heart raced, and I couldn’t sleep. I didn’t realize I was combining it with my SSRI until my therapist asked, point blank, ‘Are you taking anything else?’
Turns out, I had serotonin syndrome. Not dramatic. Not dramatic at all. Just… overwhelmed. Like my nervous system was screaming. I spent three days in a quiet room with IV fluids and a nurse who didn’t judge me.
I’m not mad at the herb. I’m mad at myself for thinking ‘natural’ meant ‘no consequences.’
Thank you for writing this. I needed to hear it again.
Wow what a wild ride this article is
so hyperforin turns on enzymes sure ok
but like did anyone actually die from this or is this just a long list of hypotheticals and scare stats
also why is the FDA even involved in herbal stuff
imagine if we regulated every plant that affects liver enzymes
green tea kills chemo drugs too guess what we dont ban green tea
also i took this for 3 years with my blood pressure med and i aint dead
so maybe stop scaring people and start asking them what they actually take
ps i still take it
pps your grammar is perfect but your logic is kinda messy