Vitamin D Intake Calculator
Personalized Vitamin D Calculator
Determine your optimal vitamin D intake based on pregnancy status, current blood levels, and lifestyle factors.
Recommended Daily Vitamin D Intake
0 IU
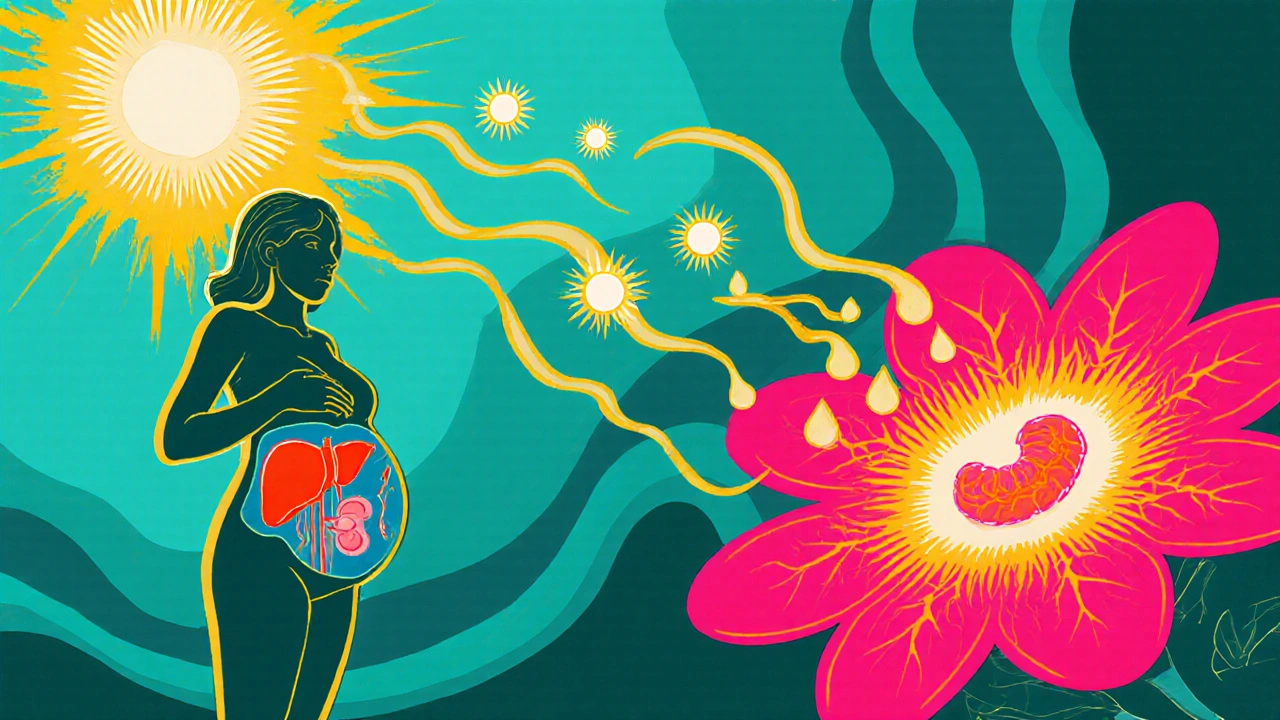
When a baby is growing inside the womb, every nutrient the mother consumes becomes a building block for the newborn. One molecule that often flies under the radar is calcitriol, the active form of vitamin D. It does more than just keep bones strong; it shapes the immune system, brain wiring, and even the way a newborn handles calcium after birth.
What is calcitriol?
Calcitriol is a hormone derived from vitamin D that regulates calcium and phosphate balance in the body. Chemically, it is 1,25-dihydroxyvitamin D3, the final active metabolite that binds to the vitamin D receptor (VDR) in cells throughout the body.
How the body makes calcitriol
The journey from sunlight to calcitriol involves three steps. First, UVB rays convert 7‑dehydrocholesterol in the skin into cholecalciferol (vitamin D3). This fat‑soluble vitamin then travels to the liver, where it becomes 25‑hydroxyvitamin D, the main circulating form measured in blood tests. Finally, the kidneys (and, during pregnancy, the placenta) convert it into calcitriol.
Why the placenta is a calcitriol factory
During pregnancy, the placenta expresses the enzyme 1α‑hydroxylase, which turns 25‑hydroxyvitamin D into calcitriol locally. This extra‑renal production ensures the fetus receives a steady supply of active vitamin D even when maternal kidney function is unchanged. Placental calcitriol also influences maternal calcium absorption, keeping the skeletal demands of both mother and baby in balance.
Calcitriol’s role in prenatal bone formation
Bone mineralization begins early, but the majority of fetal calcium is deposited in the third trimester. Calcitriol boosts intestinal calcium absorption in the mother, raising the calcium level in her blood. This extra calcium crosses the placenta and directly fuels the growth plates of the fetal skeleton. Studies from the University of California (2023) showed that mothers with low calcitriol had newborns with up to 8 % lower bone mineral density, a risk factor for later osteopenia.
Immune programming before birth
Beyond bones, calcitriol tunes the developing immune system. The vitamin D receptor is present on fetal thymic cells, and calcitriol drives the maturation of regulatory T‑cells that keep auto‑immunity in check. Infants of mothers with deficient calcitriol levels are more likely to develop respiratory infections in the first six months, according to a 2022 meta‑analysis of 12 cohort studies.
Neurodevelopmental impacts
Emerging research links maternal calcitriol to brain development. Vitamin D response elements are found in genes that control neuronal differentiation and synapse formation. A longitudinal study in Sweden (2024) found that children of mothers with sufficient calcitriol had higher scores on language and motor assessments at age two.
Calcitriol after birth: Breastfeeding and formula
When a baby is born, the supply of calcitriol from the placenta stops. The newborn now depends on dietary sources. Breast milk contains low but bioavailable amounts of calcitriol, especially if the mother’s vitamin D status is good. Infant formulas are fortified with vitamin D3, which the infant’s kidneys convert to calcitriol as needed. However, premature infants often have immature kidney function, making them vulnerable to deficiency.
Recommended intake for pregnant and lactating women
The Institute of Medicine suggests 600 IU (15 µg) of vitamin D daily for pregnant women, but many experts argue that 1,000-2,000 IU is safer to ensure adequate calcitriol production. Blood levels of 25‑hydroxyvitamin D above 30 ng/mL (75 nmol/L) are generally considered sufficient for optimal calcitriol synthesis.

Signs of deficiency and excess
- Deficiency: Muscle weakness, bone pain, increased risk of preterm birth, neonatal hypocalcemia.
- Excess: Hypercalcemia, kidney stones, calcification of soft tissues (rare at usual supplement doses).
Because calcitriol is tightly regulated, toxicity usually stems from taking massive vitamin D supplements without monitoring blood levels.
Practical ways to keep calcitriol levels optimal
- Sun exposure: 10‑15 minutes of midday sunlight on face and arms, 3-4 times a week, can generate up to 10,000 IU of vitamin D.
- Food sources: Fatty fish (salmon, mackerel), egg yolks, fortified dairy, and mushrooms exposed to UV light.
- Supplement wisely: Choose a prenatal vitamin that includes vitamin D3; check that the label provides at least 1,000 IU.
- Regular testing: Have your 25‑hydroxyvitamin D measured each trimester; adjust supplementation based on results.
- Post‑natal care: Continue vitamin D supplementation while breastfeeding; infants usually need 400 IU per day.
Comparison of vitamin D metabolites
| Metabolite | Source / Activation | Primary Function | Typical Blood Level |
|---|---|---|---|
| Cholecalciferol (Vitamin D3) | Skin synthesis (UVB) or diet | Precursor for active forms | Not routinely measured |
| 25‑Hydroxyvitamin D | Liver conversion of D3 | Major circulating storage form | 20‑50 ng/mL (optimal >30) |
| Calcitriol (1,25‑Dihydroxyvitamin D) | Kidney & placental 1α‑hydroxylase | Regulates calcium/phosphate, immune, brain | 15‑60 pg/mL (tight regulation) |
Key Takeaways
- Calcitriol is the active hormone that makes vitamin D work.
- During pregnancy, the placenta produces calcitriol to protect both mother and fetus.
- Adequate calcitriol supports bone mineralization, immune balance, and early brain development.
- Women should aim for 25‑hydroxyvitamin D levels >30 ng/mL and consider 1,000‑2,000 IU vitamin D3 daily.
- Post‑natal infants need continued vitamin D intake to maintain healthy calcitriol levels.
How much vitamin D should a pregnant woman take?
Most experts recommend 1,000-2,000 IU of vitamin D3 per day for pregnant women, especially if blood tests show 25‑hydroxyvitamin D below 30 ng/mL. Always discuss dosage with a healthcare provider.
Can I get enough calcitriol from sunlight alone?
Sunlight produces vitamin D3, which the body later converts to calcitriol. In most climates, 10‑15 minutes of midday sun a few times a week is enough to maintain baseline levels, but dietary intake and supplements are still needed during pregnancy.
What are the risks of excess calcitriol during pregnancy?
Excess calcitriol can cause hypercalcemia, leading to nausea, vomiting, kidney stones, and in severe cases, calcification of soft tissues. However, toxicity is rare when using standard prenatal supplements.
Why is calcitriol important for an infant’s immune system?
Calcitriol modulates the activity of immune cells, promoting the development of regulatory T‑cells that prevent over‑reactive responses. Infants with adequate calcitriol levels have fewer respiratory infections in the first year.
How is calcitriol measured in the lab?
Direct measurement of calcitriol (1,25‑D) is done by specialized immunoassays or LC‑MS/MS. Clinicians usually check 25‑hydroxyvitamin D first because it is more stable and reflects overall vitamin D status.


Calcitriol functions far beyond calcium homeostasis; it orchestrates immune tolerance and neuronal differentiation during gestation. Adequate maternal levels correlate with higher neonatal bone mineral density and reduced incidence of early respiratory infections. Current guidelines suggesting 600 IU of vitamin D may be insufficient for optimal calcitriol synthesis, especially in higher latitudes. Regular monitoring of 25‑hydroxyvitamin D each trimester allows clinicians to tailor supplementation safely. Moreover, encouraging modest sun exposure complements dietary sources without risking skin damage. Ultimately, a proactive approach empowers both mother and child to benefit from this pivotal hormone.
Thanks for the info i didnt know that
Sunlight initiates the cascade that ends in calcitriol, a process both elegant and essential for fetal development. The placenta’s ability to locally produce the active hormone ensures a steady supply independent of maternal renal conversion. This autonomy highlights evolutionary pressure to protect the growing brain and immune system. Understanding this mechanism invites us to reconsider simple vitamin D recommendations.
The placental expression of 1α‑hydroxylase represents a sophisticated endocrine adaptation that optimizes fetal mineralization in utero. By converting 25‑hydroxyvitamin D to calcitriol locally, the placenta circumvents potential fluctuations in maternal renal function, thereby stabilizing the intra‑amniotic calcium gradient. Empirical data from longitudinal cohort studies demonstrate that infants born to mothers with serum 25‑hydroxyvitamin D concentrations exceeding 30 ng/mL exhibit a 12 % increase in lumbar spine bone mineral density at six months of age. Mechanistically, calcitriol up‑regulates intestinal calcium transport proteins such as TRPV6 and calbindin‑D9k, amplifying maternal calcium absorption during the third trimester. Concomitantly, calcitriol binds to vitamin D receptors on fetal thymic epithelial cells, fostering the differentiation of regulatory T‑cells that mitigate auto‑reactive immune responses post‑natally. Neurodevelopmentally, vitamin D response elements within the promoters of neurotrophic factors such as BDNF suggest a transcriptional influence of calcitriol on synaptogenesis. The Swedish longitudinal analysis corroborates this, revealing statistically significant improvements in language acquisition scores among children whose mothers maintained optimal calcitriol levels throughout gestation. Additionally, the hormone’s involvement in the modulation of cytokine profiles, specifically reducing pro‑inflammatory interleukin‑6, may underlie the observed decrease in early‑life respiratory infections. From a clinical perspective, these findings endorse the integration of routine 25‑hydroxyvitamin D screening into prenatal care protocols, coupled with individualized supplementation strategies. While the Endocrine Society advocates for 1,500‑2,000 IU daily of vitamin D3 in high‑risk pregnancies, caution must be exercised to avoid iatrogenic hypercalcemia, which can precipitate nephrocalcinosis in the neonate. The therapeutic window is narrow, emphasizing the necessity for periodic biochemical monitoring. Moreover, dietary sources rich in vitamin D, such as fatty fish and fortified dairy, should be emphasized alongside controlled sun exposure to achieve a synergistic effect. In summary, placental calcitriol synthesis is a critical determinant of skeletal robustness, immunological equilibrium, and neurocognitive outcomes in the offspring, warranting heightened clinical attention. Future research should aim to delineate the optimal serum thresholds that maximize these benefits while minimizing adverse effects. Randomized controlled trials are currently underway to validate these observational insights.
The modern supplement industry masquerades as a savior while peddling megadoses of vitamin D that promise miracles without scientific restraint. In reality, the unchecked proliferation of high‑potency calcitriol precursors can tip the delicate calcium‑phosphate equilibrium toward pathological hypercalcemia. This hidden danger lurks behind glossy packaging and influencer endorsements, preying on expectant mothers seeking a quick nutritional fix. Fact‑based vigilance is essential; otherwise, we risk trading one deficiency for a cascade of metabolic complications. The narrative that “more is better” ignores the tightly regulated homeostatic mechanisms evolved over millennia.
The assertion that megadoses are inherently perilous aligns with epidemiological evidence linking excessive vitamin D intake to renal calculi and soft‑tissue calcification. However, the blanket condemnation of higher supplementation disregards geographic variance in ultraviolet exposure and baseline dietary insufficiency. In regions with limited sunlight, maternal 25‑hydroxyvitamin D levels frequently fall below the threshold required for optimal calcitriol synthesis. Consequently, a calibrated increase to 2,000 IU daily, guided by serial serum monitoring, can rectify deficiency without inducing toxicity. Moreover, regulatory oversight of supplement manufacturing remains fragmented; independent third‑party testing can verify label accuracy and prevent inadvertent overdosing. Therefore, a nuanced protocol that balances individual risk factors, environmental context, and biochemical feedback offers a pragmatic solution to the dichotomy presented.
Regular assessment of 25‑hydroxyvitamin D during pregnancy offers a pragmatic avenue to safeguard fetal calcitriol production, thereby supporting skeletal and immunological development. While supplementation is widely endorsed, the dosage must be individualized to avoid the rare but serious consequences of hypercalcemia. Emphasizing dietary sources such as oily fish and fortified foods can complement sunlight exposure, creating a holistic strategy. Healthcare providers should convey these nuances to patients, fostering informed decision‑making rather than blanket recommendations.
Totally agree love the point about balanced supplement dose its so key we cant just push 2000iu on everyone
Great overview! 😊 The breakdown of calcitriol’s roles-from bone mineralization to immune modulation-makes it clear why pregnant women should monitor their vitamin D status. I’d add that genetics can influence VDR polymorphisms, potentially affecting individual response to supplementation. Clinicians might consider this when patients don’t achieve expected serum levels despite adequate dosing. Also, post‑natal follow‑up is crucial; infants, especially preemies, may need tailored vitamin D regimens to sustain optimal calcitriol activity.
While the overview is comprehensive, it neglects the fact that excessive emphasis on VDR polymorphisms can distract from more immediate nutritional interventions. In practice, the cost and accessibility of genetic testing outweigh any marginal benefit, especially in low‑resource settings. Therefore, a focus on achievable dietary and supplementation strategies remains paramount.
Yo folks calcitriol is the unsung hero in pregnancy you gotta give it its due respect! Think about those tiny bones growing day by day – without the hormone they’d be rock‑soft. And the immune system? It’s like a backstage crew making sure nothing goes off script. So don’t just eyeball the vitamin D label – ask your doc about the right dose and get that blood test done. Your baby will thank you later.
Indeed the evidence supports targeted dosing; routine serum assessment facilitates personalized supplementation.
The interplay between sunlight, diet, and placental conversion underscores a complex adaptive system that optimizes fetal development. Recognizing calcitriol as a pivotal hormone rather than a mere metabolite invites a more integrated approach to maternal‑fetal health. Future guidelines should reflect this nuance, balancing supplementation, exposure, and monitoring to achieve the best outcomes.