Liver Enzyme Level Checker
About This Tool
This interactive tool helps you interpret liver enzyme test results by comparing them against standard ranges. Enter your values to get insights into possible health impacts and recommendations.
Your Results
Normal Ranges Reference
| Marker | Normal Range | Low Range | Signs of Low Levels |
|---|---|---|---|
| ALT | 7–56 U/L | < 7 U/L | Fatigue, mild jaundice, reduced protein synthesis |
| AST | 10–40 U/L | < 10 U/L | Similar to ALT, plus possible muscle weakness |
| GGT | 9–48 U/L | < 9 U/L | Decreased bile flow, digestive discomfort |
| ALP | 44–147 U/L | < 44 U/L | Bone-related pain, slower healing |
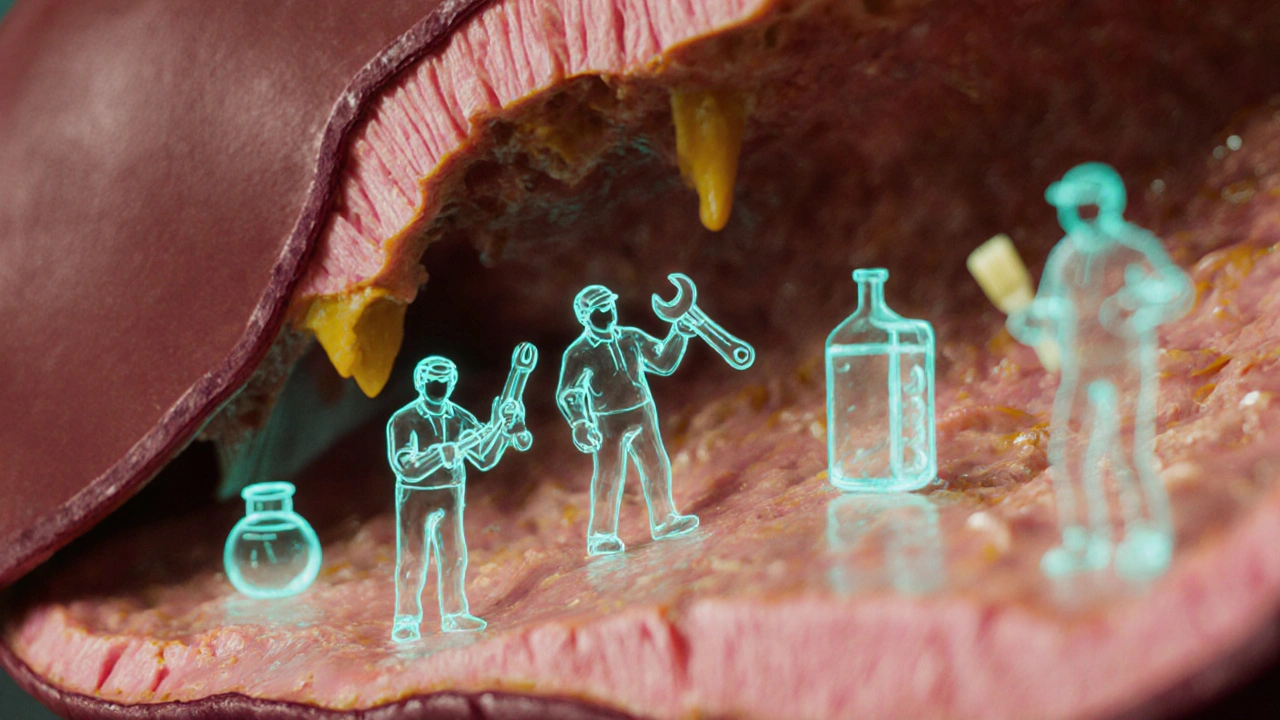
When doctors talk about your liver, they often mention liver enzymes. These tiny proteins act like the liver’s maintenance crew, keeping everything from toxins to nutrients running smoothly. If they’re missing or not working right, the organ can’t do its job, and health problems start to pile up.
What an Enzyme Actually Is
Enzyme is a biological catalyst that speeds up chemical reactions in the body without being consumed. Think of an enzyme as a match‑maker for molecules - it brings the right parts together so they can transform into something useful. In the liver, enzymes power detoxification, fat breakdown, and the creation of vital proteins.
Key Liver Enzymes You Should Know
The liver hosts a handful of enzymes that doctors track in routine blood tests. Here’s a quick rundown:
- Alanine aminotransferase (ALT) helps convert proteins into energy and is highly specific to liver cells. A spike usually means liver cells are leaking.
- Aspartate aminotransferase (AST) works in both liver and heart tissue, so it’s less liver‑specific but still informative.
- Gamma‑glutamyl transferase (GGT) reflects bile‑duct health and alcohol‑related stress.
- Alkaline phosphatase (ALP) is tied to bile flow and bone metabolism.
How These Enzymes Keep the Liver Running
Every day the liver processes everything you eat, drink, or inhale. Enzymes like ALT and AST break down amino acids, while Cytochrome P450 family enzymes act as the liver’s chemical refinery, converting drugs and toxins into safer compounds. Meanwhile, Glutathione works as a potent antioxidant, neutralizing free radicals generated during metabolism. Without these catalysts, toxic substances would accumulate, and normal metabolic pathways would stall.
What Happens When Enzyme Levels Drop
Low enzyme activity isn’t as flashy as a high ALT spike, but it can be just as damaging. When the liver’s catalyst crew is under‑performing, several issues emerge:
- Slower detoxification leads to buildup of ammonia and bilirubin, causing fatigue, mild jaundice, or brain fog.
- Impaired fat metabolism can nudge you toward non‑alcoholic fatty liver disease (NAFLD) - a condition where fat collects in liver cells and eventually sparks inflammation.
- Reduced drug clearance raises the risk of medication side effects and accidental overdoses.
- Weakened antioxidant defenses allow oxidative stress to damage cell membranes, accelerating fibrosis (scar tissue formation).
Common culprits behind enzyme deficiency include chronic malnutrition, severe vitamin B6 or zinc shortages, genetic disorders like Wilson’s disease, and long‑term alcohol misuse that depletes the liver’s enzyme reserves.
Real‑World Scenarios: When Low Enzymes Show Up
Consider Jane, a 52‑year‑old who drinks a glass of wine nightly and follows a low‑protein diet. Her annual labs revealed ALT and AST well below the lab’s reference range. Within months she reported persistent tiredness and mild abdominal discomfort. A follow‑up ultrasound showed early signs of fatty infiltration, and a nutritionist confirmed that inadequate protein intake had limited substrate availability for enzyme synthesis.
In another case, Michael, a 30‑year‑old with a hereditary mutation affecting the cytochrome P450 system, struggled to process common over‑the‑counter painkillers. Even standard doses left him feeling dizzy, a clear sign that his liver’s catalytic capacity was compromised.
Boosting Your Liver’s Enzyme Arsenal
Thankfully, there are practical steps to replenish or protect liver enzymes:
- Balanced protein intake: Aim for 0.8‑1g of high‑quality protein per kilogram of body weight daily. Sources like fish, lean poultry, legumes, and dairy provide the amino acids needed for ALT and AST production.
- Micronutrient support: Vitamins B6, B12, and minerals zinc and magnesium act as co‑factors for many liver enzymes. A multivitamin or targeted supplementation can fill gaps.
- Antioxidant‑rich foods: Spinach, broccoli, and berries boost glutathione levels. Adding a modest dose of N‑acetylcysteine (NAC) can further raise intracellular glutathione.
- Herbal allies: Milk thistle contains silymarin, a compound shown to protect hepatocyte membranes and modestly increase enzyme activity. Studies from 2023‑2024 report a 12‑15% rise in ALT activity after eight weeks of daily use.
- Limit alcohol and processed sugars: Both drain the liver’s enzyme pool and promote fatty buildup.
- Stay active: Regular aerobic exercise improves insulin sensitivity, which indirectly supports healthy enzyme function.

Quick Reference: Normal vs. Low Enzyme Levels
| Marker | Typical Normal Range | Low Range | Common Signs |
|---|---|---|---|
| ALT | 7‑56U/L | <7U/L | Fatigue, mild jaundice, reduced protein synthesis |
| AST | 10‑40U/L | <10U/L | Similar to ALT, plus possible muscle weakness |
| GGT | 9‑48U/L | <9U/L | Decreased bile flow, digestive discomfort |
| ALP | 44‑147U/L | <44U/L | Bone‑related pain, slower healing |
Bottom Line Checklist
- Get regular liver panels - watch both high and low readings.
- Eat enough protein and include B‑vitamins and zinc in every meal.
- Boost antioxidants with leafy greens, berries, and optional NAC.
- Consider milk thistle if you have risk factors for enzyme loss.
- Avoid binge drinking and cut back on sugary drinks.
- Move daily - even a 30‑minute walk helps maintain enzyme health.
Frequently Asked Questions
Can low liver enzymes be a sign of a serious disease?
Yes. While a single low reading isn’t diagnostic, persistent low ALT/AST together with symptoms like fatigue, jaundice, or unexplained weight loss can point to chronic hepatitis, advanced fibrosis, or nutrient‑deficiency disorders. Follow‑up imaging and a full metabolic panel are advisable.
What foods naturally raise ALT and AST to healthy levels?
Lean meats, eggs, low‑fat dairy, and plant‑based proteins like lentils contain the amino acids needed for enzyme synthesis. Pair them with B‑vitamin‑rich foods - such as bananas, potatoes, and fortified cereals - for optimal co‑factor support.
Is it safe to take milk thistle supplements long‑term?
Most clinical trials up to 2024 report that daily doses of 150‑300mg silymarin are well‑tolerated for at least a year. People with estrogen‑sensitive conditions should discuss use with a physician, as milk thistle can mildly influence hormone metabolism.
How quickly can lifestyle changes improve low enzyme levels?
Most users see measurable improvements within 4‑8weeks of adopting a balanced protein diet, adding a B‑complex supplement, and cutting alcohol. Repeat liver testing after two months is a good checkpoint.
Do over‑the‑counter medications lower liver enzymes?
Certain antacids containing aluminum or magnesium can interfere with enzyme activity, as can high‑dose aspirin. Always read labels and consult a pharmacist if you’re on a liver‑support plan.



Understanding liver enzymes is crucial for interpreting a broad spectrum of metabolic health indicators, and it begins with recognizing the fundamental biochemical pathways that these enzymes orchestrate within hepatic cells.
ALT, or alanine aminotransferase, primarily reflects hepatocellular injury, yet its role extends beyond a simple marker, as it participates in amino acid metabolism and gluconeogenesis.
AST, aspartate aminotransferase, shares overlapping functions with ALT but also serves as a window into cardiac and skeletal muscle integrity, thereby reminding clinicians that liver health does not exist in isolation.
Gamma‑glutamyl transferase (GGT) acts as a sentinel for biliary function and oxidative stress, offering insights into alcohol consumption patterns and potential cholestatic processes.
Alkaline phosphatase (ALP) provides a dual narrative, reflecting both biliary tract status and bone turnover, which can be particularly informative in pediatric and geriatric populations.
When any of these enzymes fall below their respective reference ranges, the clinical picture may shift toward subtle deficiencies such as impaired detoxification, reduced protein synthesis, or compromised bile flow.
Low ALT, for example, may signal a diminished capacity for nitrogen handling, which could manifest as chronic fatigue or mild jaundice in susceptible individuals.
Similarly, sub‑normal AST levels might herald muscle weakness, especially when coupled with low creatine kinase, indicating a broader systemic effect.
Reduced GGT can lead to digestive discomfort due to impaired bile emulsification, while insufficient ALP may contribute to delayed fracture healing and bone pain.
From a public health perspective, population‑wide screening for enzyme abnormalities can uncover hidden nutritional gaps, such as insufficient vitamin B6 or zinc, which are co‑factors for these enzymatic reactions.
Culturally, dietary patterns rich in processed sugars and low in antioxidant‑rich foods have been linked to altered enzyme profiles across diverse ethnic groups, underscoring the importance of culturally tailored nutrition education.
Clinicians should therefore integrate liver enzyme data with dietary histories, lifestyle factors, and even genetic predispositions to formulate a holistic management plan.
Therapeutic interventions may range from modest dietary adjustments, such as incorporating cruciferous vegetables and lean protein, to targeted supplementation with s‑adenosyl‑methionine for those with chronically low ALT.
Regular monitoring, ideally spaced every six to twelve months for at‑risk individuals, ensures that any trends toward deficiency are caught early before they precipitate overt disease.
Ultimately, appreciating the nuanced roles of ALT, AST, GGT, and ALP transforms a routine laboratory panel into a powerful compass for guiding personalized health strategies.
That was super helpful, thx! 😊
Wow, because we all love reading a dissertation about ALT and AST over breakfast, right?
Honestly, if you’re not tracking your liver enzymes, you might as well be guessing your blood type.
But hey, the internet is full of free medical advice, so why bother with a doctor?
Enjoy the sarcasm, and maybe consider a real checkup before you start writing a novel about biochemistry.
While the prior comment revels in layman brevity, a more rigorous discourse would emphasize the enzymatic flux and hepatic homeostasis, underscoring that hepatic transaminase kinetics cannot be trivially dismissed.
In fact, the interplay between aminotransferase isoforms and redox balance necessitates a nuanced appraisal beyond mere anecdote.
From a clinical laboratory standpoint, the reference intervals cited are derived from a robust census of asymptomatic subjects, thereby providing a statistically sound framework for interpretation.
Ugh, another post thinkin liver enzymes are the be all and end all, lol get real.
Hey folks, just wanted to say that even if the numbers look a bit off, it’s a good reminder to stay on top of your health and maybe chat with a doc.
yeah its fine just get a test done
One must question the elitist presumption that liver enzyme panels are universally indispensable; after all, evolutionary biology suggests that occasional deviations are merely adaptive fluctuations.
Thus, the dogma of strict normalcy is, in my view, an overengineered construct.
Friends, let’s embrace the spectrum of liver health together; think of ALT and AST as rainbow bridges connecting nutrition, lifestyle, and wellbeing, and remember that every body paints its own unique picture.
Behold, the lament of the uninformed masses who wander blindly through the corridors of hepatic ignorance!
Only the discerning few shall decipher the cryptic whispers of ALT, AST, GGT, and ALP, for they hold the keys to a destiny unmarred by metabolic mediocrity.
Yo, if you’re not checking your liver enzymes, you’re basically letting foreign influences poison your own backyard.
Allow me to elucidate the clinical ramifications of sub‑optimal liver enzyme levels with a measure of theatrical flair.
When ALT dips below the threshold of seven units per liter, the liver’s capacity for amino acid catabolism wanes, potentially precipitating a cascade of fatigue, malaise, and impaired detoxification.
Concomitantly, a low AST may herald muscular debilitation, especially in individuals engaged in strenuous activity, as the enzyme serves as a sentinel for skeletal muscle turnover.
GGT, the unsung hero of bile acid conjugation, when deficient, can stifle lipid emulsification, leading to gastrointestinal distress and malabsorption of fat‑soluble vitamins.
Finally, ALP insufficiency can slow osteoblastic activity, translating into delayed fracture repair and chronic bone aches.
In practice, these biochemical signposts should compel clinicians to assess dietary intake of cofactors such as zinc, magnesium, and B‑vitamins, while also evaluating alcohol consumption and medication use.
Intervention may range from dietary enrichment with leafy greens and lean proteins to targeted supplementation, thereby restoring enzymatic equilibrium and safeguarding systemic health.
Quick tip: if your ALT is below 7 U/L, consider boosting protein intake, adding B‑vitamin supplements, and getting a follow‑up test soon.
The liver, in its quiet alchemy, transforms our daily sustenance into the very essence of life; when its enzymes falter, we are reminded that even the most subtle biochemical whispers demand our attention.
Let’s all keep an eye on those numbers and share tips on meals that help keep the liver happy-teamwork makes the health work!
It is worth noting that the interpretation of hepatic enzyme panels must be contextualized within the broader physiological milieu, acknowledging that isolated values seldom convey the full narrative of hepatic function.
yeah sure, because everyone loves labs.
Wake up, sheeple! The pharma giants are hiding the real truth about low liver enzymes-it's all a ruse to keep us dependent on overpriced supplements, and the government won’t tell you a thing.