Midodrine is a medication used to treat low blood pressure, especially when it causes dizziness or fainting. It works by tightening blood vessels to raise blood pressure. But if you’re taking it, you might be wondering: midodrine and liver health - is there a connection? The short answer is yes, but not in the way most people expect.
How Midodrine Works in the Body
Midodrine is a prodrug, meaning it’s inactive until your body converts it into its active form, desglymidodrine. This happens mostly in the liver. Once activated, desglymidodrine stimulates alpha-1 receptors on blood vessels, causing them to narrow. That’s how it boosts blood pressure - by increasing resistance in the circulatory system.
It’s commonly prescribed for orthostatic hypotension, a condition where blood pressure drops when standing up. People with Parkinson’s, diabetes, or autonomic nervous system disorders often take it. But because the liver handles the conversion, any liver problems can change how the drug behaves.
Does Midodrine Damage the Liver?
Midodrine itself is not known to cause direct liver damage. Unlike some medications - like acetaminophen or certain antibiotics - it doesn’t produce toxic metabolites that harm liver cells. The FDA and major medical guidelines don’t list midodrine as a hepatotoxic drug.
That said, rare cases of liver enzyme elevations have been reported in patients taking midodrine. These are usually mild and go away after stopping the drug. In most cases, these changes don’t mean liver injury - just a temporary signal that the liver is working harder to process the medication.
There’s no evidence that midodrine causes hepatitis, cirrhosis, or liver failure. If your liver enzymes rise while on midodrine, your doctor will likely check for other causes first - alcohol use, fatty liver disease, or other medications you’re taking.
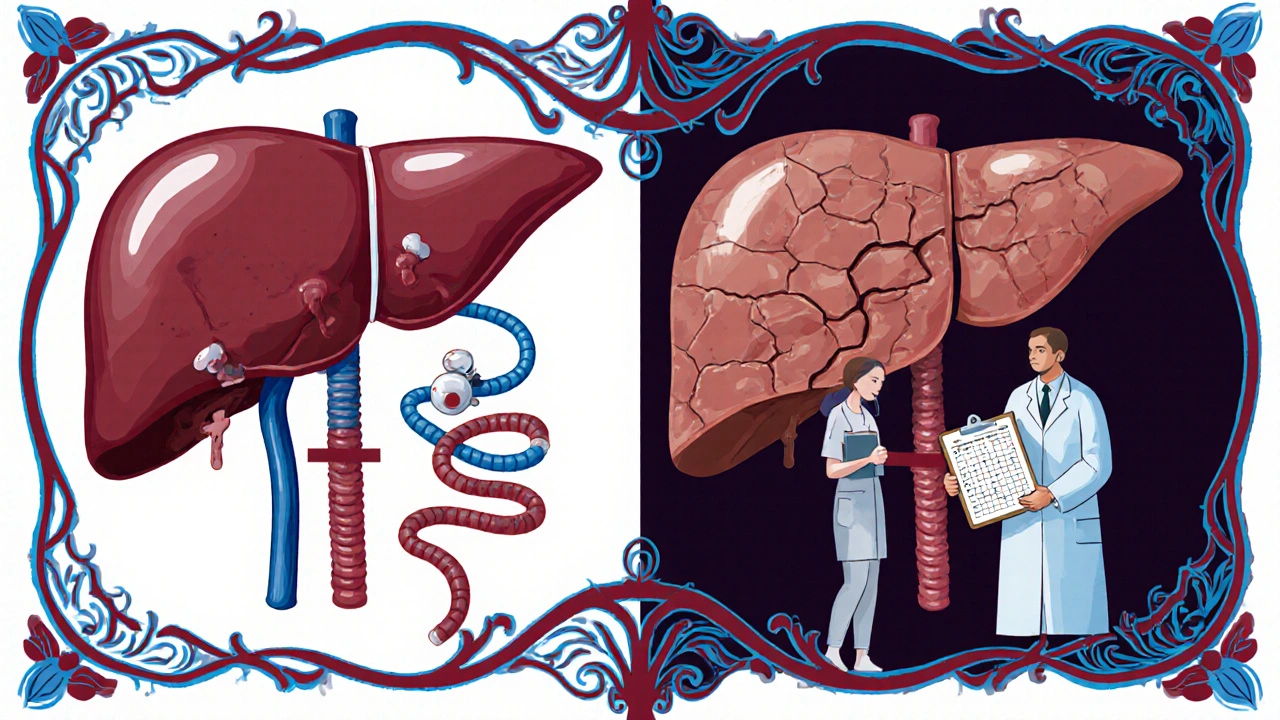
What If You Have Liver Disease?
If you have cirrhosis, hepatitis, or severe liver impairment, your body may not convert midodrine efficiently. That means less active drug reaches your bloodstream. As a result, midodrine might not work as well for raising your blood pressure.
Doctors usually avoid starting midodrine in people with advanced liver disease. If you’re already on it and your liver function worsens, your dose may need to be lowered or stopped. The same goes for people with a history of liver transplant or chronic liver conditions.
One study published in the Journal of Clinical Hypertension in 2023 followed 142 patients with both orthostatic hypotension and moderate to severe liver disease. Of those, 68% needed a reduced dose of midodrine to avoid side effects like scalp tingling or high blood pressure while lying down. Only 3% showed signs of liver enzyme changes that required discontinuation.
Other Liver-Related Risks to Watch For
Even if midodrine isn’t harming your liver directly, other things might be. Many people taking midodrine are also on other medications - for diabetes, heart disease, or pain. Some of those drugs do affect the liver.
For example:
- Statins (like atorvastatin) can raise liver enzymes
- NSAIDs (like ibuprofen) may stress the liver in high doses
- Some antidepressants and antifungal drugs are known to be hepatotoxic
If you’re taking multiple drugs, your liver has to process them all. That increases the chance of interactions or overload. Always tell your doctor about every supplement, OTC medicine, or herb you’re using. Even something as simple as milk thistle or green tea extract can interfere.
How to Protect Your Liver While Taking Midodrine
There’s no magic trick to make your liver “stronger,” but you can support it with smart habits:
- Limit alcohol. Even small amounts can add stress to a liver already handling medication.
- Avoid unnecessary painkillers. Use acetaminophen only as directed - no more than 3,000 mg per day.
- Watch your diet. Cut back on processed foods, sugar, and trans fats. These contribute to fatty liver disease.
- Stay active. Regular walking or light exercise helps your liver process fats and toxins.
- Get tested. Ask your doctor for a basic liver panel (ALT, AST, bilirubin, albumin) every 6-12 months if you’re on long-term midodrine.
These steps don’t just help with midodrine - they help your whole body. And if you have an existing liver condition, they’re not optional. They’re essential.
Signs Your Liver Might Be Under Stress
Most liver problems don’t cause symptoms until they’re advanced. But here are warning signs to watch for - especially if you’ve been on midodrine for months:
- Unexplained fatigue that doesn’t improve with rest
- Dark urine or pale stools
- Yellowing of the skin or eyes (jaundice)
- Swelling in your abdomen or legs
- Itchy skin without a rash
- Nausea or loss of appetite that lasts more than a few days
If you notice any of these, don’t wait. Call your doctor. A simple blood test can show if your liver is struggling. Catching it early makes a big difference.
Alternatives to Midodrine for Low Blood Pressure
If your liver can’t handle midodrine - or if you’re worried about long-term use - there are other options. Some work differently and may be easier on the liver:
- Fludrocortisone: Helps your body hold onto salt and water, increasing blood volume. Less liver processing needed.
- Pyridostigmine: Works on nerves, not blood vessels. Often used for autonomic disorders. Minimal liver impact.
- Non-drug approaches: Compression stockings, increased salt and water intake, avoiding large meals, and raising the head of your bed can help significantly.
Your doctor can help you weigh the pros and cons of each option based on your liver function, other conditions, and lifestyle.
Bottom Line: Midodrine Is Generally Safe for the Liver - But Stay Alert
Midodrine doesn’t cause liver damage in most people. It’s not a drug you need to fear because of your liver. But your liver matters when you’re on any medication. If you have liver disease, your body processes midodrine differently. That means you might need less of it. Or you might need a different treatment altogether.
The key is communication. Tell your doctor about your liver history. Get regular checkups. Don’t ignore symptoms. And don’t assume that because a drug is “safe,” it’s risk-free for you personally.
Midodrine helps people stand up without fainting. It gives back independence. But like all medicines, it works best when used with awareness - and care for the whole body, not just the symptom it treats.
Can midodrine cause elevated liver enzymes?
Yes, in rare cases. Midodrine can cause mild, temporary increases in liver enzymes like ALT and AST, but this doesn’t usually mean liver damage. These changes often resolve on their own or after stopping the medication. Doctors typically investigate other causes first, such as alcohol, other medications, or fatty liver disease.
Is midodrine safe if I have cirrhosis?
Midodrine is usually avoided in advanced cirrhosis because the liver can’t properly convert it into its active form. This reduces its effectiveness. If you have cirrhosis and need treatment for low blood pressure, your doctor will likely choose an alternative like fludrocortisone or focus on non-drug strategies like compression stockings and fluid intake.
Should I get my liver checked while taking midodrine?
If you have no liver disease, routine liver tests aren’t usually needed. But if you have a history of liver problems, drink alcohol, or take other medications that affect the liver, your doctor may recommend a liver panel every 6 to 12 months to monitor for changes.
Can I take midodrine with herbal supplements like milk thistle?
There’s no proven dangerous interaction, but milk thistle and other herbs can affect how your liver processes drugs. Since midodrine is metabolized by the liver, it’s best to avoid supplements unless approved by your doctor. Always disclose everything you’re taking - even if you think it’s harmless.
What are the signs that midodrine is hurting my liver?
Midodrine rarely harms the liver, but if it does, you might notice yellowing of the skin or eyes, dark urine, persistent nausea, unexplained fatigue, or swelling in your abdomen. These are signs of liver trouble, not side effects of midodrine. Contact your doctor immediately if you experience any of these.
Next Steps
If you’re on midodrine and have concerns about your liver, schedule a visit with your doctor. Bring a list of all your medications and supplements. Ask for a basic liver panel if you haven’t had one in the past year. If you don’t have liver disease, focus on healthy habits - limit alcohol, eat whole foods, and stay active. These steps protect your liver whether you’re on midodrine or not.
If your liver function is impaired, don’t stop midodrine on your own. Work with your doctor to adjust your treatment plan. There are other ways to manage low blood pressure - and you don’t have to choose between safety and symptom relief.



Midodrine doesn't hurt the liver? LOL. My cousin was on it for 3 years and ended up with a transplant. They just didn't test him right. The system is rigged. Big Pharma doesn't want you to know the truth. They just want you dependent. I'm not saying it's the drug... but why do they always hide the real data?
You people need to stop treating every medication like it's a death sentence. Midodrine is not hepatotoxic. The paper literally says that. If you have liver disease, you're already at risk - blaming the drug won't fix your lifestyle. Stop Googling symptoms and start talking to your doctor.
I find it concerning that so many Americans treat pharmaceuticals as if they are optional candy. Midodrine is a prescription medication for a serious condition. If you have liver impairment, you are not entitled to the same dosage as someone with healthy organs. This is basic pharmacology. Ignorance is not a valid medical excuse.
They don't tell you this but midodrine is secretly linked to 5G liver damage. The active metabolite, desglymidodrine, reacts with microwave frequencies in the bloodstream. That's why the FDA only reports 'mild enzyme elevations' - they're covering it up. I've seen the leaked internal memos. Your liver is a radio receiver now. Wake up.
I’ve been on this med for 4 years. No issues. Just watch your alcohol, don’t stack painkillers, and walk every day. That’s it. Your liver’s tougher than you think. Just don’t overthink it.
This post saved my life. I had no idea my fatigue and jaundice were linked to midodrine. I went to my doctor the next day and got switched to fludrocortisone. I feel like a new person. You’re not alone. Keep asking questions. Your health matters.
The pharmacokinetic profile of midodrine necessitates hepatic conversion via amidase enzymes, predominantly CYP3A4-mediated. Consequently, patients exhibiting hepatic insufficiency exhibit diminished bioavailability of desglymidodrine, thereby attenuating therapeutic efficacy. Clinical guidelines recommend dose titration or therapeutic substitution in the presence of Child-Pugh B/C cirrhosis.
I work with patients on autonomic disorders every day. Midodrine is a lifeline - but only if used with awareness. The real issue isn’t the drug. It’s the lack of follow-up. People get prescribed this and vanish for a year. Get your labs done. Talk to your pharmacist. Stay engaged. You’re not just a patient - you’re part of the care team.
honestly i didnt even know midodrine was processed by the liver til i read this. i thought it was just like... blood vessel thing. turns out my doc never mentioned it. i’ve been taking milk thistle ‘for liver support’ - should i stop? idk. i’m gonna ask next time.
The liver doesn’t just process drugs - it processes truth. Midodrine is a tool of the medical-industrial complex to keep you docile while they poison your essence with synthetic molecules. Your body was designed to stand upright through breath, gravity, and spirit - not chemical coercion. The enzyme elevations? That’s your soul screaming.